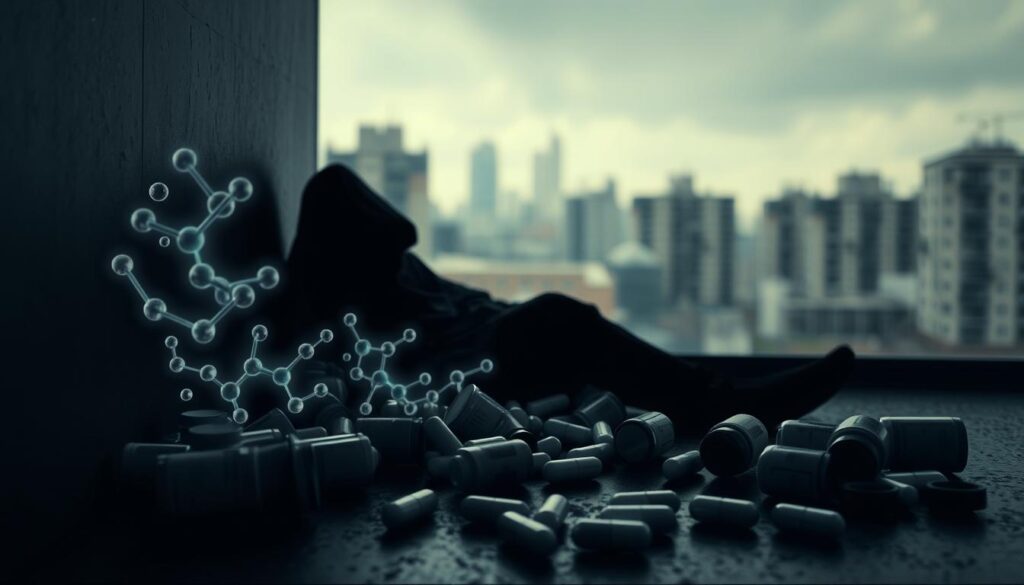
Xylazine, a non-opioid sedative, poses a critical public health threat in illegal drug supplies. This dangerous substance, not approved for human use, is often mixed with fentanyl1. The combination, known as “tranq dope,” can be lethal1.
The DEA reports widespread xylazine presence across the United States. In 2022, it was found in 23% of seized fentanyl powder and 7% of fentanyl pills1. Xylazine has now infiltrated illegal drugs in 48 out of 50 states1.
This trend highlights severe health risks associated with xylazine and opioid effects2. Overdose deaths involving xylazine have risen dramatically. Between 2015 and 2020, there was a nearly 20-fold increase in major US regions2.
The White House has labeled xylazine an emerging threat. Its devastating impact has worsened the ongoing opioid crisis.
Key Takeaways
- Xylazine is a non-FDA-approved sedative found in illegal drug supplies
- The substance is commonly mixed with fentanyl, increasing overdose risks
- DEA reports xylazine presence in drugs across nearly all U.S. states
- Overdose deaths involving xylazine have increased dramatically
- This drug presents severe health risks beyond typical opioid effects
Understanding Xylazine: Origins and Uses
Xylazine is a powerful synthetic chemical with a complex history. It was developed in 1962 for medical and veterinary use. This substance has found important applications beyond its initial research purposes.
Understanding its origins sheds light on its current role. It has significant uses in both medical and veterinary practices.
What is Xylazine?
Xylazine is a potent alpha2-adrenergic agonist mainly used in veterinary medicine. It acts as a sedative, muscle relaxant, and pain reliever for animals.
Its medical applications are specific. However, researchers have noted potential risks related to xylazine abuse and side effects3.
Common Medical Applications
The primary uses of xylazine include:
- Sedation for large animals
- Pain management in veterinary settings
- Muscle relaxation during medical procedures
- Anesthetic support for surgical interventions
Xylazine in Veterinary Medicine
Veterinarians rely on xylazine for managing animal health. Its rapid onset and long duration make it valuable for complex treatments.
Interestingly, xylazine’s presence in drug samples has increased dramatically3:
| Location | Xylazine Prevalence | Year |
|---|---|---|
| New York City | 2.2% of syringes | 2017 |
| Philadelphia | 91% of drug samples | Recent Years |
| Connecticut | Overdose deaths doubled | 2019-2020 |
Understanding xylazine’s complex nature requires careful examination of its medical and potential misuse implications.
Xylazine’s growing presence in various regions is concerning. It calls for more research and awareness about its potential side effects and abuse risks4.
The Opioid Crisis: A Brief Overview
The opioid epidemic is a critical national emergency in the United States. It has devastating effects on individuals, families, and communities. Effective intervention strategies are crucial to address this public health challenge.
Devastating Overdose Statistics
The opioid crisis has reached alarming levels. In 2022, opioids were involved in 76% of nearly 108,000 drug overdose deaths5.
Since 1999, opioid overdose deaths have increased tenfold5. Each day, an average of 224 people die from opioid overdoses5.
Key Trends in Opioid-Related Deaths
- Synthetic opioid deaths increased by around 4%5
- Heroin overdose deaths decreased by 36%5
- Prescription opioid overdose deaths dropped by approximately 12%5
Efforts to Address Opioid Addiction
Early detection of opioid overdose symptoms is vital to prevent fatal outcomes. Medical experts and community groups are developing comprehensive addiction treatment approaches.
“Our goal is to save lives and provide hope for those struggling with addiction.” – Public Health Expert
| Year | Opioid Overdose Deaths | Key Developments |
|---|---|---|
| 1999 | Low baseline | Initial rise in opioid prescriptions |
| 2022 | 108,000 total overdose deaths | Increased focus on prevention |
The Centers for Disease Control and Prevention (CDC) supports states in fighting this epidemic5. They collect data, identify outbreaks, and provide comprehensive care.
The CDC aims to reduce the impact of opioid addiction on communities nationwide. Their efforts are crucial in combating this widespread health crisis.
How Xylazine Interacts with Opioids
Xylazine and opioids form a deadly mix, posing a serious threat in today’s drug scene. This dangerous combo carries huge risks that everyone should know about6.
Mechanisms of Neurological Interaction
Xylazine is a strong central nervous system depressant. It makes opioids even more dangerous when combined. This mix creates a deadly synergy, greatly raising overdose risks6.
- Causes profound sedation
- Dramatically slows respiratory function
- Reduces brain oxygen levels
- Eliminates natural protective physiological responses
Synergistic Brain Effects
Xylazine and opioids together cause complex brain issues. Studies show this mix stops the normal rise in brain oxygen seen with opioids alone6.
| Substance | Primary Effect | Overdose Risk |
|---|---|---|
| Opioids Alone | Respiratory Depression | High |
| Xylazine + Opioids | Extreme Respiratory Suppression | Critically High |
The mixture of xylazine and opioids represents an escalating public health emergency that demands immediate attention and comprehensive intervention strategies.
Many users take this risky mix without knowing it. Some areas see a big jump in xylazine deaths. The U.S. government now calls this combo an emerging drug threat7.
Knowing these complex interactions helps people grasp the deadly risks. The xylazine-opioid mix is a serious danger that needs urgent action6.
Signs and Symptoms of Xylazine Use
Recognizing xylazine use warning signs is vital for effective opioid abuse prevention. Early detection can lead to timely intervention and potentially save lives.
Physical Symptoms to Watch For
Xylazine side effects show up as distinct physical indicators. These can be quite alarming for users and observers.
- Severe sedation and extreme drowsiness8
- Respiratory depression with slow breathing8
- Unusual skin ulcers and open wounds8
- Decreased heart rate8
- Low blood pressure8
Behavioral Changes Indicating Use
Behavioral shifts can also point to potential xylazine use. Keep an eye out for these warning signs:
- Persistent confusion and disorientation8
- Difficulty maintaining consciousness8
- Memory problems8
- Sudden mood shifts8
Early detection of these symptoms can be critical in preventing potential overdose and supporting recovery.
Xylazine-related overdose deaths have surged alarmingly. The rate jumped from 0.36 percent in 2015 to 6.7 percent in 20209.
This increase highlights the need to understand xylazine’s side effects. It also stresses the importance of strong opioid abuse prevention strategies.
| Symptom Category | Specific Indicators |
|---|---|
| Physical Symptoms | Skin ulcers, slow breathing, low blood pressure |
| Behavioral Changes | Confusion, drowsiness, memory issues |
| Overdose Risk | High when combined with opioids or alcohol |
If you suspect a xylazine-related health emergency, act fast. Contact emergency medical services right away8.
The Risks of Combining Xylazine with Opioids
Xylazine and opioids create a deadly mix, posing severe health risks. This combination challenges medical treatments and can be fatal. Users face grave dangers when mixing these substances.
Short-Term Risks of Xylazine and Opioid Interaction
Xylazine with opioids amplifies dangers significantly. From January 2019 to June 2022, fentanyl deaths involving xylazine surged by 276%10.
Short-term risks include:
- Increased risk of fatal overdose
- Severe respiratory depression
- Rapid loss of consciousness
- Unpredictable drug interactions
Long-Term Health Consequences
Xylazine and opioids together cause serious health issues. In the South, xylazine-positive overdose deaths skyrocketed by 1,127%11.
Long-term users may face:
| Health Consequence | Potential Impact |
|---|---|
| Skin Ulceration | Severe wound development requiring medical intervention |
| Infection Risk | Increased susceptibility to dangerous skin infections |
| Withdrawal Complexity | Compounded symptoms of multiple substance dependencies |
Healthcare providers must remain vigilant. Narcan can reverse opioid effects, even with xylazine present. However, these complex interactions require specialized medical care11.
“Understanding the risks is the first step in preventing devastating consequences.” – Drug Safety Expert
Treatment Options for Xylazine Dependency
Xylazine abuse requires a multi-faceted approach. It tackles both physical and mental aspects of addiction. The treatment landscape has evolved to meet challenges posed by this dangerous drug combo.
Successful recovery involves various strategies. These support individuals through tough withdrawal processes. They also aid in long-term rehabilitation.
Behavioral Therapies
Behavioral interventions are key in treating xylazine abuse. They help people understand their addiction triggers. These approaches also teach healthier coping methods.
- Cognitive Behavioral Therapy (CBT)
- Motivational Interviewing
- Group Counseling Sessions
- Individual Psychological Support
Medication-Assisted Treatments
Managing xylazine withdrawal needs special medical care. Doctors often suggest specific drugs to address complex symptoms.
| Medication | Purpose | Effectiveness |
|---|---|---|
| Clonidine | Withdrawal Symptom Management | High |
| Benzodiazepines | Anxiety and Muscle Relaxation | Moderate |
| Dexmedetomidine | Withdrawal Symptom Reduction | Promising |
Doctors note that xylazine withdrawal can be very tough. Users say it’s often more painful than regular opioid withdrawal12. Experts stress the need for complete treatment plans.
These plans should address both physical and mental aspects of dependency13. A holistic approach is key for effective treatment.
Effective treatment requires a holistic approach that combines medical intervention, psychological support, and ongoing care.
Doctors suggest reducing stigma for those seeking help. Creating supportive environments is crucial for xylazine and opioid addiction treatment14. Comprehensive strategies make recovery more achievable for those struggling with addiction.
Legal Status of Xylazine in the U.S.
Xylazine’s legal status in the U.S. is complex. It’s not federally controlled, but its presence in illicit drugs is growing. Xylazine poses unique challenges in opioid addiction treatment1.
Current Regulatory Approach
Xylazine isn’t a federally controlled substance. However, states are taking action to address its impact. Several have classified it as a controlled substance.
- Ohio classified xylazine as a Schedule III controlled substance15
- Pennsylvania initiated proceedings to temporarily classify it as a Schedule III drug15
- West Virginia passed Senate Bill 546 to classify xylazine as a Schedule IV drug15
Comparison with Controlled Substances
Xylazine abuse prevention faces unique hurdles. The DEA has found xylazine and fentanyl mixtures in 48 states1. In 2022, xylazine was present in 23% of fentanyl powder and 7% of fentanyl pills seized1.
Drug enforcement agencies are worried about xylazine’s role in the opioid crisis. The White House has declared fentanyl mixed with xylazine an emerging threat1.
Emerging Detection and Monitoring
States are implementing advanced strategies to combat xylazine abuse. These include allowing drug checking equipment and expanding surveillance programs.
- 22 states and Washington D.C. permit drug checking equipment15
- Eight additional states allow specific testing for synthetic opioids15
- States like Maryland, Massachusetts, and North Carolina have expanded drug supply surveillance programs15
Xylazine remains a complex regulatory challenge. Awareness and proactive measures are key to addressing its risks in opioid addiction treatment.
Addressing Misconceptions About Xylazine
Xylazine is a dangerous drug additive causing confusion about its effects and risks. Understanding these misconceptions is vital for public safety and effective intervention strategies.
Xylazine’s presence in the drug supply poses significant dangers. Clear information about this substance is crucial for developing appropriate responses.
Debunking Common Myths About Xylazine
Many people have wrong ideas about xylazine and its role in substance use. The DEA found xylazine mixed with fentanyl in 48 out of 50 states16.
This shows how widespread the problem has become. It’s important to separate fact from fiction when discussing xylazine.
- Myth: Naloxone is completely ineffective against xylazine overdoses
- Reality: While naloxone doesn’t reverse xylazine’s specific effects, it remains critical in treating opioid components of an overdose
- Myth: All xylazine users develop visible skin wounds
- Reality: Skin ulcers are common but not universal among users
Understanding Xylazine in Substance Use
Xylazine misuse has serious consequences. In Philadelphia, xylazine detection in drug-related deaths rose from less than 2% to over 31%16.
A Chicago study found fentanyl present in 99.1% of xylazine-associated deaths16. This shows how often xylazine is combined with other dangerous drugs.
“Many individuals using xylazine-laced drugs are unaware of its presence in their substance supply.” – Public Health Expert
Xylazine misuse is more than just a health risk. It’s a major public health challenge that needs careful study and targeted action.
| Misconception | Actual Facts |
|---|---|
| Xylazine is harmless | Highly dangerous when mixed with opioids |
| All users develop same symptoms | Varied individual health impacts |
| Easy to detect in drug supply | Often undetectable without specialized testing |
Knowing these details about xylazine can help communities fight back. Better understanding leads to more effective prevention and treatment strategies.
Community Impact: How Xylazine Affects Society
Xylazine has created major challenges for North American communities. It requires a new approach to opioid abuse prevention. Emergency services and community groups are working to understand and address this dangerous substance.
The Role of Emergency Services
Emergency responders face new challenges with xylazine-related incidents. Xylazine-involved overdose rates have increased 12-fold between 2018 and 2021 in the USA17. The drug presents unique problems for first responders.
- Xylazine cannot be reversed with naloxone
- Rescue breathing and CPR are critical in overdose situations18
- Requires specialized training for emergency personnel
Support Resources for Families
Families affected by xylazine use need comprehensive support. Education and understanding are key to effective opioid abuse prevention strategies.
| Support Resource | Type of Assistance |
|---|---|
| Community Counseling Centers | Emotional Support |
| Addiction Recovery Programs | Treatment Guidance |
| Family Support Groups | Peer Counseling |
Understanding and compassion are the first steps in addressing substance use challenges.
Xylazine has spread across multiple regions in the USA. It started in the Northeast and moved to the Rust Belt, Southern, and Western areas17.
The drug’s spread shows the need for community-based substance use prevention. Working together, communities can fight xylazine’s spread and help those affected.
The Future of Xylazine in Drug Policy
Xylazine poses big challenges in opioid addiction treatment. Policymakers and researchers are tackling this dangerous substance’s impact on public health. The drug policy landscape is changing fast to address these issues.
Xylazine’s presence in the drug world is growing alarmingly. Fatal drug poisonings involving xylazine jumped from 260 to 3,480 cases between 2018 and 202119. Overdose deaths with xylazine increased 20-fold from 2015 to 2020 across major U.S. regions20.
Potential Legislative Changes
Legislators are considering multiple approaches to combat xylazine abuse:
- Scheduling xylazine as a controlled substance
- Implementing stricter controls on veterinary use
- Developing comprehensive monitoring systems
Research Directions and Future Studies
Critical research priorities include:
- Understanding long-term health impacts
- Developing effective xylazine dependency treatments
- Creating rapid detection methods
| Research Focus | Key Objectives |
|---|---|
| Toxicology | Comprehensive health effect analysis |
| Addiction Treatment | Specialized intervention strategies |
| Detection Methods | Advanced screening technologies |
Philadelphia faces a severe xylazine problem. Over 90% of street opioids there now contain this dangerous substance19. Researchers are working on xylazine test strips and exploring harm reduction strategies20.
“Our approach must be comprehensive and data-driven to effectively address this emerging public health crisis.”
Xylazine complicates opioid addiction treatment. Teamwork between policymakers, healthcare pros, and researchers is key to fighting its impact21. Their efforts will shape future strategies against this growing threat.
Conclusion: Navigating the Xylazine and Opioid Landscape
Xylazine has transformed the opioid crisis, creating new challenges for public health. Overdose rates involving xylazine have surged across North America. This indicates a rapidly evolving and increasingly dangerous drug landscape22.
Your awareness plays a vital role in fighting this epidemic. Prevention strategies must now consider xylazine’s presence in illicit drug supplies. Recent studies show a 12-fold increase in fatal xylazine-positive overdoses from 2018 to 202123.
Staying informed and prepared can make a life-saving difference. Administering naloxone remains crucial during suspected overdoses, even with xylazine present. Seek support from local health departments and addiction specialists for guidance.
Key Takeaways for the Public
Knowing the risks of xylazine and opioids is your best defense. Learn to spot the signs and remember that help is always available. Education and support are key for those facing substance use disorders.
Resources for Further Information
For more support, reach out to the National Institute on Drug Abuse. Local health departments and community harm reduction programs can also help. These resources address the changing landscape of substance abuse effectively.
FAQ
What is xylazine and why is it dangerous?
How does xylazine interact with opioids?
What are the physical symptoms of xylazine use?
Is naloxone effective against xylazine overdose?
How widespread is xylazine in the drug supply?
How is xylazine withdrawal treated?
Is xylazine a controlled substance?
What are the long-term health risks of xylazine use?
Source Links
- What You Should Know About Xylazine – https://www.cdc.gov/overdose-prevention/about/what-you-should-know-about-xylazine.html
- Xylazine: What Clinicians Need to Know – https://www.health.ny.gov/publications/12044.pdf
- PDF – https://oasas.ny.gov/system/files/documents/2023/10/xylazine-guidance.pdf
- Xylazine appears to worsen the life-threatening effects of opioids in rats – https://www.nih.gov/news-events/news-releases/xylazine-appears-worsen-life-threatening-effects-opioids-rats
- Understanding the Opioid Overdose Epidemic – https://www.cdc.gov/overdose-prevention/about/understanding-the-opioid-overdose-epidemic.html
- Xylazine appears to worsen the life-threatening effects of opioids in rats | National Institute on Drug Abuse – https://nida.nih.gov/news-events/news-releases/2023/06/xylazine-appears-to-worsen-the-life-threatening-effects-of-opioids-in-rats
- Xylazine Poisoning in Clinical and Forensic Practice: Analysis Method, Characteristics, Mechanism and Future Challenges – https://www.mdpi.com/2305-6304/11/12/1012
- Xylazine – https://www.mayoclinic.org/diseases-conditions/drug-addiction/in-depth/xylazine/art-20559909
- Xylazine Facts – SMART – https://smart.ips.tennessee.edu/smart-policy-network/policy-briefs/xylazine-facts/
- Opioids Mixed With Xylazine: Effects & Risks | Greenhouse – https://greenhousetreatment.com/opiate/laced-with-xylazine/
- ADH warns of presence of xylazine in illegal drugs – Arkansas Department of Health – https://healthy.arkansas.gov/article/adh-warns-of-presence-of-xylazine-in-illegal-drugs/
- Xylazine’s Growing Impact on Drug Use and Treatment Options | Johns Hopkins Bloomberg School of Public Health – https://publichealth.jhu.edu/2024/xylazines-growing-impact-on-drug-use-and-treatment-options
- Opioids Laced with Xylazine: Effects & Dangers | AdCare – https://adcare.com/opioids/laced-with-xylazine/
- Xylazine Toxicity – StatPearls – NCBI Bookshelf – https://www.ncbi.nlm.nih.gov/books/NBK594271/
- State and Federal Actions to Respond to Xylazine – https://www.nga.org/news/commentary/state-and-federal-actions-to-respond-to-xylazine/
- What Is Xylazine? A Medical Toxicologist Explains How It Increases Overdose Risk and Why Narcan Can Still Save a Life – https://www.scientificamerican.com/article/what-is-xylazine-a-medical-toxicologist-explains-how-it-increases-overdose-risk-and-why-narcan-can-still-save-a-life1/
- Public health impact and harm reduction implications of xylazine-involved overdoses: a narrative review – Harm Reduction Journal – https://harmreductionjournal.biomedcentral.com/articles/10.1186/s12954-023-00867-x
- Colorado Department of Public Health and Environment – https://cdphe.colorado.gov/overdose-prevention/xylazine
- The emerging fentanyl–xylazine syndemic in the USA: challenges and future directions – https://pmc.ncbi.nlm.nih.gov/articles/PMC10842070/
- Xylazine and Drug Mixtures – https://store.samhsa.gov/sites/default/files/xylazine-drug-mixtures-pep24-02-015.pdf
- PDF – https://www.pharmacy.ohio.gov/xylazine
- Potency-Enhancing Synthetics in the Drug Overdose Epidemic: Xylazine (“Tranq”), Fentanyl, Methamphetamine, and the Displacement of Heroin in Philadelphia and Tijuana | Journal of Illicit Economies and Development – https://jied.lse.ac.uk/articles/10.31389/jied.122
- Public health impact and harm reduction implications of xylazine-involved overdoses: a narrative review – https://pmc.ncbi.nlm.nih.gov/articles/PMC10498612/