Breast cancer surgery can be tough. Knowing about mastectomy is vital for patients facing this diagnosis. It’s a surgery that removes breast tissue to prevent or treat breast cancer1.
There are two main types of breast cancer surgery. These include total (simple) mastectomy and modified radical mastectomy1. Your treatment plan may involve different ways to remove lymph nodes and rebuild the breast.
Some patients choose immediate reconstruction during mastectomy. This often gives better cosmetic results1. Women with specific genetic mutations might consider risk-reducing mastectomy as prevention1.
Breast reconstruction isn’t required after mastectomy. Some people opt for breast prosthesis or flat closure12. The surgery process carefully considers many factors. These include possible lymph node involvement and individual health conditions.
Key Takeaways
- Mastectomy is a comprehensive breast cancer surgery option
- Multiple reconstruction approaches are available
- Genetic factors can influence surgical decisions
- Lymph node removal is often part of the procedure
- Patient choice plays a significant role in treatment
What is a Mastectomy: Types and Purpose
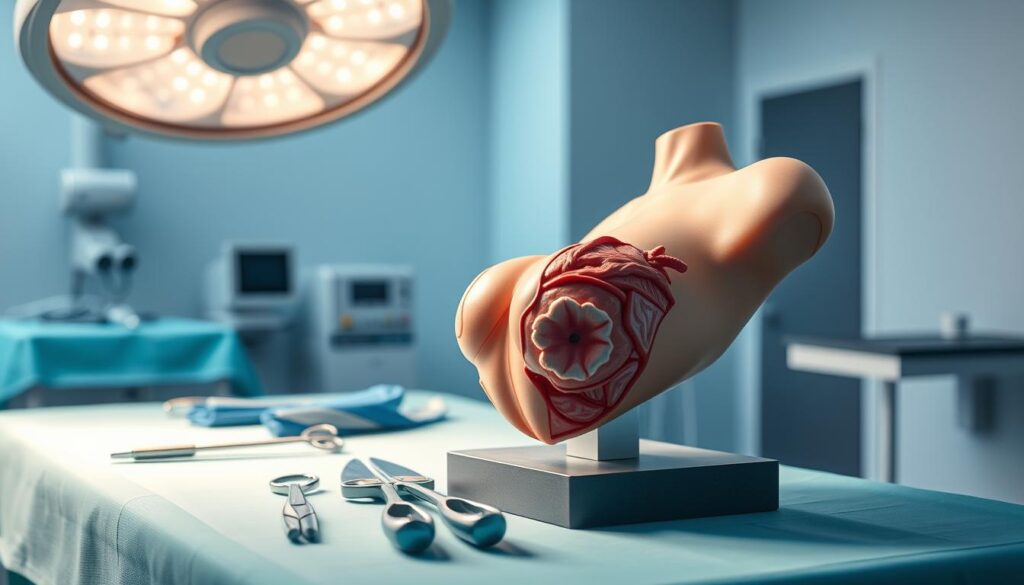
Mastectomy is a crucial surgery for breast cancer treatment. It removes breast tissue to prevent or treat cancer. There are several approaches tailored to individual medical needs3.
Mastectomy techniques offer various levels of tissue removal and reconstruction possibilities. Your healthcare team will help you choose the best approach for your condition4.
Total (Simple) Mastectomy
A total mastectomy removes the entire breast, including tissue, nipple, and areola. It’s typically recommended for specific conditions.
- Ductal Carcinoma In Situ (DCIS)
- Paget disease with underlying DCIS
- Invasive breast cancer
- Prophylactic risk reduction
Modified Radical Mastectomy
The modified radical mastectomy is more extensive. It removes the entire breast, chest muscle lining, and axillary lymph nodes.
- Entire breast
- Lining of chest muscles
- Axillary lymph nodes
This approach is commonly used for invasive and inflammatory breast cancer cases4.
Skin-Sparing and Nipple-Sparing Options
Modern mastectomy techniques focus on preserving appearance while treating cancer effectively. These options can be combined with immediate breast reconstruction.
| Procedure | Skin Preservation | Nipple Preservation |
|---|---|---|
| Skin-Sparing Mastectomy | Most skin preserved | No |
| Nipple-Sparing Mastectomy | Most skin preserved | Yes |
Your surgical team will assess your case to recommend the most suitable approach5. These techniques can offer a more natural appearance4.
“The goal is not just removing cancer, but helping you feel whole and confident afterward.”
Recovery time usually ranges from 2 to 6 weeks. It depends on the specific procedure and reconstruction method5. Always discuss risks, benefits, and expected outcomes with your doctor.
Preparing for Mastectomy Surgery: Essential Steps
Mastectomy prep requires careful planning. Your medical team will guide you through pre-surgical testing. This ensures you’re fully ready for the procedure6.
During your pre-surgical consultation, you’ll share vital health info. This includes your medical history and current medications.
You’ll also discuss anesthesia concerns and potential allergies.
- Complete medical history review
- Medication management disclosure
- Current prescription and supplement details
- Anesthesia considerations and potential allergies
Lifestyle changes are key before surgery. Your doctor may suggest quitting smoking and cutting back on alcohol.
Maintaining a healthy diet is also important. These steps can improve your surgery outcome.
- Smoking cessation
- Alcohol reduction
- Maintaining a healthy diet
Fertility preservation matters for future pregnancy plans. Talk to your medical team about options early on7.
“Preparation is key to a successful surgical experience and smoother recovery.” – Breast Cancer Medical Experts
| Pre-Surgical Checklist | Important Actions |
|---|---|
| Medical Preparation | Complete all recommended tests |
| Transportation | Arrange reliable post-surgery transportation |
| Recovery Support | Prepare home for post-surgical care |
Sleep apnea needs special attention. Bring breathing devices and discuss anesthesia risks with your doctor6.
Good preparation can boost your surgery results. It also helps smooth out your recovery process8.
Recovery and Post-Mastectomy Care
Post-mastectomy recovery involves both physical and emotional healing. Understanding this process helps you navigate challenges with confidence and resilience.
Managing Physical Recovery
After mastectomy surgery, your body needs time to heal. Full recovery typically takes six to eight weeks. Most patients return to work within three to six weeks9.
Drainage Care and Wound Healing
Wound care is crucial in post-mastectomy recovery. You’ll likely have one to two surgical drains requiring careful management9.
- Empty drains at least twice daily
- Avoid showering while drains are in place
- Monitor incision areas for potential complications
Pathology results typically take 3-5 days to complete9. Patience is key during this stage.
Physical Therapy and Exercise
Rehabilitation plays a vital role in post-mastectomy recovery. Avoid strenuous activities for the first month10. Gentle exercises can help prevent lymphedema and improve mobility.
| Recovery Milestone | Recommended Action |
|---|---|
| First Week | Rest and light movement |
| 2-4 Weeks | Gentle physical therapy |
| 4-6 Weeks | Gradually increase activity |
Emotional Support and Coping Strategies
Recovery extends beyond physical healing. Family and friends’ support can significantly impact your healing process10. Consider joining support groups or seeking counseling for emotional challenges.
“Healing is not just about the body, but also the mind and spirit.”
Stay hydrated by drinking 6-8 glasses of water daily. Focus on nutritious, easy-to-digest foods9. Your journey is unique, and every step forward is a triumph.
Conclusion
Your mastectomy journey continues after surgery. Breast cancer survivorship requires ongoing care and support. Regular check-ups are vital for monitoring your health and spotting changes early11.
Your healthcare team will guide you through long-term care strategies. These plans aim to support both your physical and emotional recovery.
Understanding the psychological impact is crucial. Research shows mastectomies can be emotionally challenging, especially for young women11. Many survivors develop strong coping skills.
Support groups, counseling, and open talks with your medical team can help. These resources can guide you through this life-changing experience.
Medical advances are improving mastectomy techniques and post-op care. New methods include risk-reducing approaches12 and robotic surgery. Staying informed helps you make the best choices for your health.
A mastectomy is just one chapter in your story. It’s a testament to your strength and resilience. Embrace available support and focus on your overall recovery.
With the right resources and mindset, you can move forward confidently. Your journey of healing and hope continues beyond surgery.
FAQ
What exactly is a mastectomy?
How do I know if I need a mastectomy?
What should I do to prepare for a mastectomy?
What can I expect during recovery?
What are my breast reconstruction options?
How long does it take to recover from a mastectomy?
Will I need additional treatments after mastectomy?
How will a mastectomy affect my emotional well-being?
Source Links
- Mastectomy – https://www.komen.org/breast-cancer/treatment/type/surgery/mastectomy/
- What is a Mastectomy? – https://www.cancer.org/cancer/types/breast-cancer/treatment/surgery-for-breast-cancer/mastectomy.html
- What Is a Mastectomy? – https://my.clevelandclinic.org/health/procedures/21221-mastectomy
- Mastectomy – https://www.hopkinsmedicine.org/health/conditions-and-diseases/breast-cancer/mastectomy
- Mastectomy – https://www.facs.org/for-patients/the-day-of-your-surgery/breast-cancer-surgery/understanding-your-operation/mastectomy/
- Preparing for Breast Cancer Surgery: A Patient’s Guide to What to Expect – https://www.premiersurgicalnetwork.com/breast-cancer-surgery-preparation/
- Mastectomy – Mayo Clinic – https://www.mayoclinic.org/tests-procedures/mastectomy/about/pac-20394670
- 17 Must-Haves for Recovery after Mastectomy from Survivors – https://www.nationalbreastcancer.org/blog/checklist-for-recovery-after-mastectomy/
- PDF – https://healthcare.msu.edu/_assets/documents/surgery/mastectomy_postop_draft_LGM_20220425.pdf
- Breast Cancer Treatment Postoperative Care and Services- Brigham and Women’s Hospital – https://www.brighamandwomens.org/surgery/breast-surgery/post-operative-care
- Beyond the scars: a qualitative study on the experiences of mastectomy among young women with breast cancer in a country with crisis – https://pmc.ncbi.nlm.nih.gov/articles/PMC10641941/
- Mastectomy—A Critical Review – https://www.scirp.org/journal/paperinformation?paperid=76963