Pericardial effusion is a serious heart condition. It happens when extra fluid builds up around the heart. This can lead to major health risks if not treated1.
Many things can cause this problem. These include infections, diseases, and inflammation. Autoimmune disorders like rheumatoid arthritis can trigger it. Cancer that spreads to the heart area can also cause it1.
Chest injuries and heart surgery can lead to pericardial effusion. Radiation therapy near the heart is another possible cause. Bacterial, viral, and parasitic infections may also be to blame1.
Key Takeaways
- Pericardial effusion involves fluid buildup around the heart
- Multiple medical conditions can trigger this heart condition
- Early detection is crucial for preventing serious complications
- Treatment varies based on underlying cause and severity
- Professional medical evaluation is essential for proper diagnosis
Understanding Pericardial Effusion and Its Impact on Heart Health
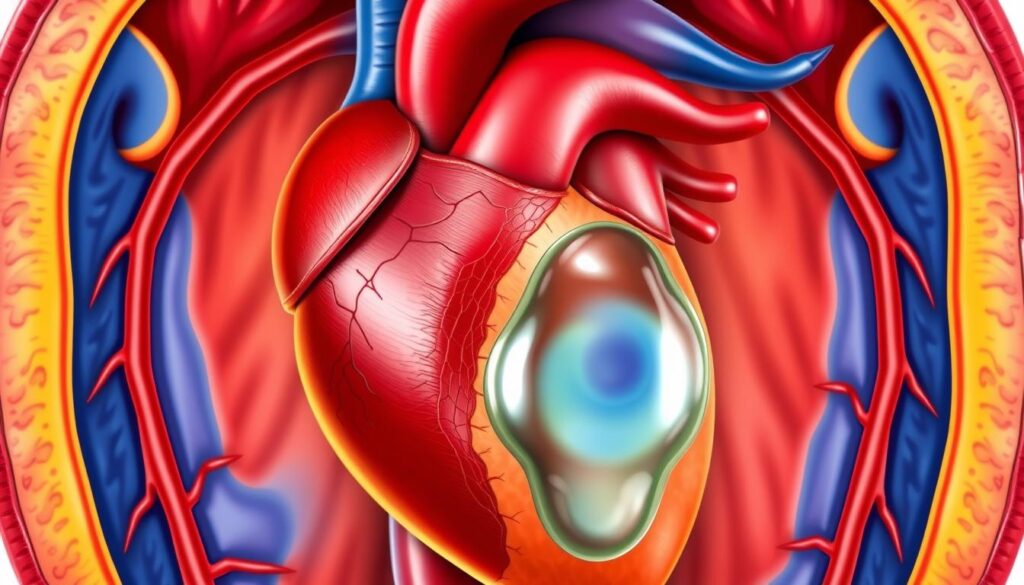
The heart’s protective membrane is vital for cardiovascular health. A small amount of fluid surrounds the heart in the pericardial cavity. This fluid affects heart function and can indicate potential health issues.
What Is the Pericardium and Normal Fluid Levels
The pericardium contains 15 to 50 milliliters of clear, yellow fluid. This fluid lubricates and protects the heart. It allows smooth heart movement and provides cushioning2.
Excess fluid can trigger a condition called pericardial effusion. This occurs when fluid levels exceed normal amounts.
How Excess Fluid Affects Heart Function
Too much fluid in the pericardial cavity can compress the heart. This compression prevents proper heart filling. It may lead to cardiac tamponade, restricting blood flow and oxygen delivery2.
Symptoms might include chest pressure, heart palpitations, and shortness of breath. These signs warrant immediate medical attention.
Risk Factors and Common Triggers
Pericardial effusion can stem from various causes:
- Infections (bacterial, viral, fungal)3
- Autoimmune disorders3
- Cancer-related complications3
- Medical treatments like chemotherapy
“Understanding the underlying causes of pericardial effusion is key to effective management and treatment.”
Recent heart surgery, chronic kidney disease, and radiation therapy increase pericardial effusion risk. Acute pericarditis, a related condition, has a 20% to 30% recurrence rate3.
| Cause Category | Percentage of Cases |
|---|---|
| Idiopathic | 55% |
| Post-Cardiac Injury | 20% |
| Infections | 14% |
| Cancer-Related | 5% |
| Autoimmune Disorders | 5% |
Echocardiograms can help detect pericardial effusion early2. This allows for effective management. Seek medical help if you experience ongoing cardiac symptoms.
Recognizing Signs and Medical Diagnosis Methods
Recognizing pericardial effusion symptoms is vital for quick treatment. Your body may signal heart sac issues. Be alert to chest pain and breathing difficulties.
- Chest discomfort or sharp pain
- Persistent shortness of breath
- Lightheadedness
- Swelling in the abdomen or legs
Doctors use various methods to confirm pericardial effusion. These techniques help identify fluid buildup causes and severity4.
- Physical examination
- Chest X-ray
- Echocardiography
- Computed Tomography (CT) scan
- Cardiac Magnetic Resonance Imaging (MRI)
European medical guidelines favor echocardiography for pericardial effusion evaluation5. This definitive evaluation method measures fluid levels and assesses heart function impacts.
“Early detection is key to preventing serious cardiac complications” – Cardiology Experts
Your doctor might suggest ECG or pericardiocentesis for thorough diagnosis. These tests help identify underlying conditions and guide treatment plans6.
Conclusion
Understanding pericardial effusion treatment options is vital. Your doctor may suggest pericardiocentesis if fluid buildup affects heart function7. Treatment depends on whether the cause is inflammatory or not7.
Pericardial effusion treatment varies by medical condition. Neoplastic causes are common7. Patients with systemic issues may need complex interventions8. Cardiac rehab can help recovery and prevent future problems.
Your medical team will create a personalized treatment plan. Patients with heart failure or lung diseases need closer monitoring8. Early detection and thorough care are crucial for managing pericardial effusion.
Every case is unique. Work closely with your doctor for the best treatment plan. Regular check-ups and following prescribed treatments are important. Participating in cardiac rehab can boost your heart health long-term.
FAQ
What is pericardial effusion?
What are the common symptoms of pericardial effusion?
What causes pericardial effusion?
How is pericardial effusion diagnosed?
What are the treatment options for pericardial effusion?
Can pericardial effusion be dangerous?
Who is at higher risk for developing pericardial effusion?
How long does recovery from pericardial effusion typically take?
Source Links
- Pericardial effusion-Pericardial effusion – Symptoms & causes – Mayo Clinic – https://www.mayoclinic.org/diseases-conditions/pericardial-effusion/symptoms-causes/syc-20353720
- Pericardial Effusion: Causes, Symptoms, and Treatment – https://www.webmd.com/heart-disease/pericardial-effusion
- Pericardial Disease Center | UCSF Cardiology – https://ucsfhealthcardiology.ucsf.edu/patient-care/clinical-services/pericardial-disease-center
- Diagnosis, treatment, and management of pericardial effusion- review – https://pmc.ncbi.nlm.nih.gov/articles/PMC9283797/
- Pericardial effusion – https://www.saem.org/about-saem/academies-interest-groups-affiliates2/cdem/for-students/online-education/m3-curriculum/bedside-ultrasonagraphy/pericardial-effusion
- Pericardial Disease – https://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/cardiology/pericardial-disease/
- Unveiling the causes of pericardial effusion in a contemporary case series of pericardiocentesis in Latin America – https://pmc.ncbi.nlm.nih.gov/articles/PMC9512803/
- Pericardial effusions and cardiac tamponade in hospitalized systemic sclerosis patients: analysis of the national inpatient sample – BMC Rheumatology – https://bmcrheumatol.biomedcentral.com/articles/10.1186/s41927-023-00360-9