Your body sends important signals. Pelvic floor dysfunction is one you shouldn’t ignore. Uterine prolapse can disrupt your daily life and overall well-being.
Pregnancy and childbirth are main causes of this condition. Vaginal deliveries may increase your risk1.
Women are more likely to experience vaginal prolapse as they age. Almost half of women aged 50-79 have some form of pelvic organ prolapse2.
Obesity, genetics, and aging can also affect your pelvic health1. Pelvic organ prolapse isn’t just one condition. It’s a range of issues that can affect women differently.
Organs may drop slightly in mild cases. In severe cases, they can descend significantly1.
Key Takeaways
- Pelvic organ prolapse is common among women, especially after childbirth
- Multiple factors contribute to pelvic floor weakness
- Symptoms can range from mild discomfort to significant physical challenges
- Early detection and management are crucial for maintaining quality of life
- Lifestyle changes can help manage pelvic floor health
What is Pelvic Organ Prolapse and Its Impact on Women’s Health
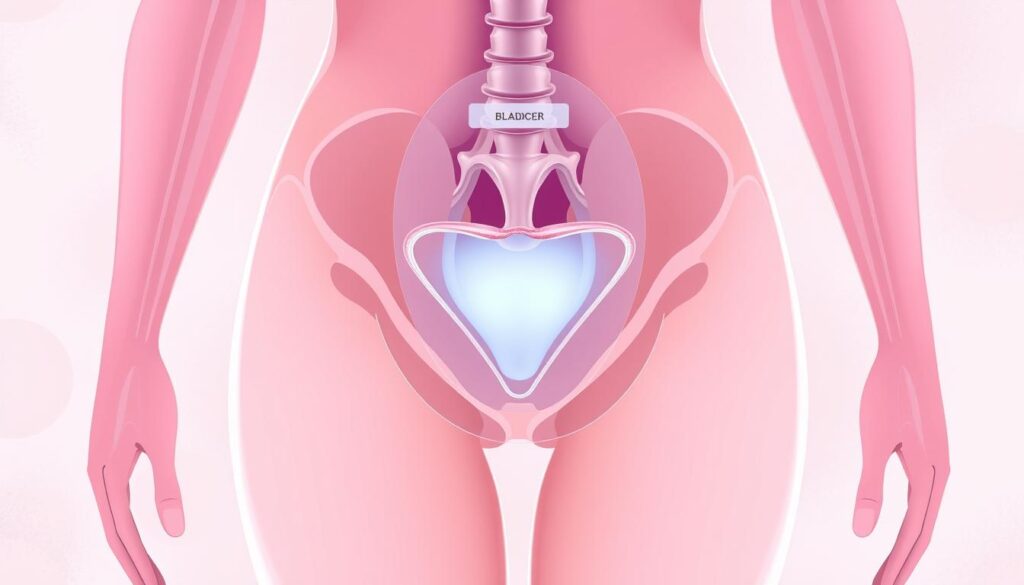
Pelvic organ prolapse (POP) affects millions of women worldwide. It occurs when pelvic floor muscles weaken, causing internal organs to descend. This can lead to discomfort and health issues3.
Understanding the Condition
POP happens when pelvic muscles lose strength. This causes organs like the bladder, uterus, or rectum to drop. It can appear as cystocele, rectocele, uterine prolapse, or vaginal vault prolapse4.
Common Symptoms and Warning Signs
- Feeling of pressure or fullness in the pelvic area
- Visible bulge near the vaginal opening
- Difficulty with urination or bowel movements
- Lower back pain
- Uncomfortable sexual intercourse
Different Types of Pelvic Organ Prolapse
The primary types of pelvic organ prolapse include:
- Cystocele: Bladder dropping into the vaginal canal
- Rectocele: Rectum bulging into the vaginal wall
- Uterine prolapse: Uterus descending into the vaginal canal
- Vaginal vault prolapse: Top of the vagina dropping after hysterectomy
Risk Factors and Contributing Conditions
Several factors can increase your chance of developing pelvic organ prolapse. Childbirth, especially multiple vaginal deliveries, is a major contributor5.
Other risk factors include:
- Aging and menopause
- Obesity
- Chronic coughing
- Heavy lifting
- Genetic predisposition
“Understanding your body and early detection are key to managing pelvic organ prolapse effectively.”
One in four women in their 40s experience some form of pelvic organ prolapse. This increases to one in three for women in their 60s3.
Stay informed and proactive about your pelvic health. This can help you manage and potentially prevent this condition.
Comprehensive Treatment Options for Pelvic Support
Pelvic organ prolapse offers multiple treatment paths. Your recovery depends on condition severity and personal health factors6. Various approaches aim to provide relief and restore pelvic floor functionality.
Pelvic floor therapy is a primary conservative treatment strategy. Specialists recommend supervised muscle training for at least 16 weeks6. Kegel exercises help regain muscle control and reduce prolapse symptoms.
- Lifestyle modifications
- Pelvic floor exercises
- Pessary devices
- Surgical interventions
Pessary devices offer a non-surgical solution for moderate to severe prolapses6. These silicone devices provide structural support and prevent organ displacement7. They’re ideal if you’re avoiding surgery or planning future pregnancies.
| Treatment Option | Benefits | Considerations |
|---|---|---|
| Pelvic Floor Therapy | Muscle strengthening | Requires consistent practice |
| Pessary Devices | Non-surgical support | May require periodic replacement |
| Surgical Intervention | Permanent correction | Longer recovery period |
Surgical treatments become necessary when conservative methods fall short8. Reconstructive surgeries repair weak pelvic floor areas and reposition organs. Procedures like sacrocolpopexy and colporrhaphy address different types of pelvic organ prolapse8.
“Your treatment journey is unique, and the right approach depends on your individual health needs and lifestyle.” – Pelvic Health Specialist
Each treatment option has potential side effects. Consult a healthcare professional to make an informed decision tailored to your situation6.
Advanced Surgical Solutions and Recovery Journey
Pelvic reconstructive surgery offers hope for women with pelvic organ prolapse. These advanced solutions can greatly improve your life quality. Innovative medical approaches make this possible.
Reconstructive Procedure Options
Surgical interventions become crucial when conservative treatments fail. The main reconstructive procedures include:
- Sacrocolpopexy: A gold standard technique that suspends the vaginal vault using surgical mesh9. This procedure has an impressive success rate of 80-90% in treating advanced pelvic organ prolapse9.
- Colporrhaphy: A surgical method that reinforces vaginal walls to support bladder and rectum positioning.
- Sacrohysteropexy: A procedure that lifts the uterus using surgical mesh attached to specific anatomical points.
Comprehensive Surgical Approach
Surgical options depend on each patient’s unique needs. About 37% of women with pelvic floor disorders are 60-79 years old10.
Your surgeon will consider age, previous childbirths, and overall health. These factors help determine the best reconstructive technique for you.
| Procedure | Success Rate | Recovery Time |
|---|---|---|
| Sacrocolpopexy | 80-90% | 4-6 weeks |
| Colporrhaphy | 75-85% | 3-5 weeks |
Recovery and Expectations
Post-surgery recovery needs patience and careful management. You’ll likely spend 2-3 days in the hospital and 4-6 weeks off work9.
For the first eight weeks, avoid heavy lifting, aerobic exercises, and sex. Slowly increase activity as your doctor recommends9.
Your surgical journey is unique, and successful recovery depends on following medical guidance and maintaining a positive outlook.
These procedures have low complication rates. Pain during sex and mesh exposure occur in 2-3% of cases9.
Talk to your doctor about possible risks and pain management. This helps ensure the best outcome for you11.
Conclusion
Pelvic organ prolapse impacts women globally, with rates from 1-65%12. Early detection and personalized care can greatly enhance your life quality. Research shows that proactive management is key to handling this condition effectively.
Start by making lifestyle changes to prevent prolapse. Try targeted exercises, maintain a healthy weight, and avoid straining your pelvic floor13. Work with healthcare pros to create a care plan that fits your unique needs.
Women aged 50-59 face the highest risk of symptomatic pelvic organ prolapse12. Being proactive about pelvic floor care is crucial. Treatment options vary from exercises to surgery, based on your symptoms13.
Stay informed and listen to your body. Seek expert advice to manage pelvic organ prolapse effectively. Your path to better pelvic health is personal and empowering.
FAQ
What exactly is pelvic organ prolapse?
What are the most common symptoms of pelvic organ prolapse?
Who is most at risk for developing pelvic organ prolapse?
What treatment options are available for pelvic organ prolapse?
Can pelvic organ prolapse be prevented?
How long is the recovery process for pelvic organ prolapse surgery?
Are there different types of pelvic organ prolapse?
Is pelvic organ prolapse a serious condition?
Source Links
- Understanding Pelvic Organ Prolapse – https://www.acog.org/womens-health/videos/understanding-pelvic-organ-prolapse
- Pelvic Organ Prolapse – https://www.uclahealth.org/medical-services/womens-pelvic-health/conditions-treated/pelvic-organ-prolapse
- 5 Things I Wish All Women Knew About Pelvic Organ Prolapse – https://www.acog.org/womens-health/experts-and-stories/the-latest/5-things-i-wish-all-women-knew-about-pelvic-organ-prolapse
- Pelvic organ prolapse – Symptoms and causes – https://www.mayoclinic.org/diseases-conditions/pelvic-organ-prolapse/symptoms-causes/syc-20360557
- Pelvic Organ Prolapse | Continence Foundation of Australia – https://www.continence.org.au/who-it-affects/women/prolapse
- Pelvic organ prolapse – Treatment – https://www.nhs.uk/conditions/pelvic-organ-prolapse/treatment/
- Pelvic organ prolapse – Diagnosis and treatment – https://www.mayoclinic.org/diseases-conditions/pelvic-organ-prolapse/diagnosis-treatment/drc-20562951
- What To Know About Pelvic Organ Prolapse – https://my.clevelandclinic.org/health/diseases/24046-pelvic-organ-prolapse
- Sacrocolpopexy (Pelvic Organ Prolapse Surgery) | CU Urogynecology – https://urogyn.coloradowomenshealth.com/treatments/pelvic-reconstructive-surgery/sacrocolpopexy.html
- Pelvic Organ Prolapse – https://www.draliabadi.com/gynecology/vaginal-conditions/pelvic-organ-prolapse/
- My journey with pelvic organ prolapse – https://www.bswhealth.com/blog/my-journey-with-pelvic-organ-prolapse
- Pelvic organ prolapse: The lived experience – https://pmc.ncbi.nlm.nih.gov/articles/PMC9629641/
- Pelvic organ prolapse | RCOG – https://www.rcog.org.uk/for-the-public/browse-our-patient-information/pelvic-organ-prolapse/