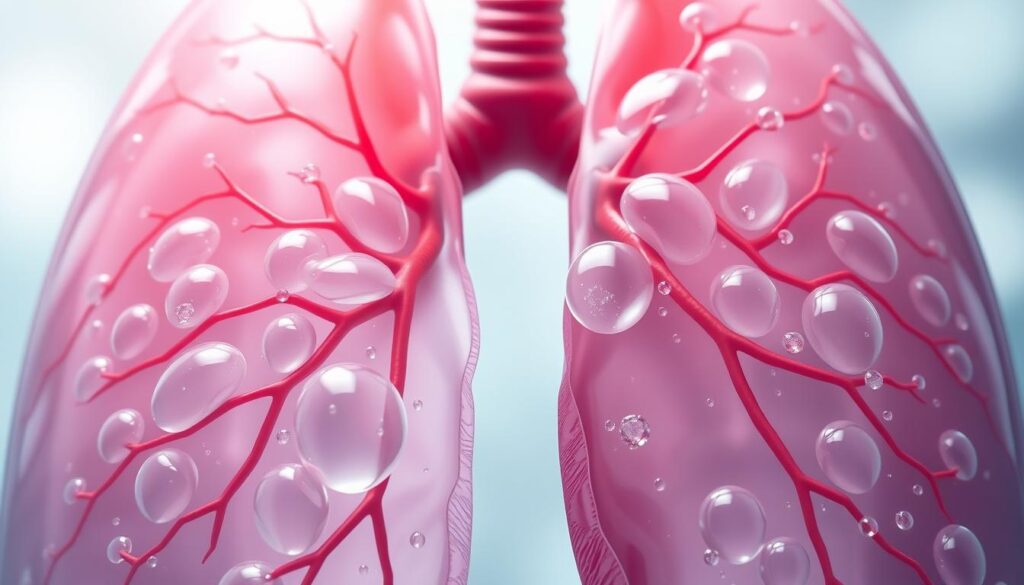
Lung fluid buildup is a serious condition that affects your breathing and health. Pulmonary edema happens when fluid fills the lungs’ air sacs1. This makes it hard to breathe and get enough oxygen.
Heart issues are the main cause of this dangerous problem. Various medical conditions can lead to fluid in your lungs1. Heart failure and coronary artery disease often increase pressure and fluid buildup1.
Other factors can also cause pulmonary edema. These include pneumonia, toxins, certain medications, and high altitudes1. Knowing these risks helps with early detection and quick treatment.
Key Takeaways
- Pulmonary edema is a critical condition affecting lung function
- Heart problems are the most common underlying cause
- Symptoms can range from mild to life-threatening
- Immediate medical attention is essential
- Multiple factors can contribute to lung fluid accumulation
Understanding Pulmonary Edema and Its Impact on Breathing
Pulmonary edema is a serious lung condition. It causes fluid buildup in the lungs’ air sacs. This disrupts normal breathing and oxygen exchange2.
With pulmonary edema, lungs struggle to exchange gases. This leads to severe symptoms like dyspnea. Dyspnea makes breathing extremely difficult3.
How Normal Lung Function Works
Healthy lungs work like complex breathing machines. Alveoli, tiny air sacs, transfer oxygen into the blood. They also remove carbon dioxide efficiently.
In pulmonary edema, these sacs fill with fluid. This blocks proper gas exchange. It also causes crepitations during breathing4.
Types of Pulmonary Edema
- Cardiogenic pulmonary edema (heart-related)
- Noncardiogenic pulmonary edema (non-heart-related)
Heart failure often causes cardiogenic pulmonary edema. It forces fluid into lung tissues. Noncardiogenic causes include ARDS, drug reactions, and high-altitude exposure2.
Risk Factors and Common Causes
Certain conditions increase your risk of pulmonary edema. Key risk factors include:
- Heart diseases
- Kidney problems
- High-altitude travel
- Chronic health conditions
Fluid buildup can lead to hypoxemia. Early detection and treatment are crucial. Knowing these risks helps you spot warning signs quickly3.
Critical Warning Signs and Symptoms to Watch For
Spotting pulmonary edema signs could save your life. This serious condition has critical symptoms needing immediate medical care. Your body signals when breathing becomes difficult.
Key symptoms you should never ignore include:
- Severe shortness of breath (dyspnea), especially when lying down
- Feeling like you’re drowning or suffocating
- Coughing up pink, frothy sputum5
- Rapid or irregular heartbeat
- Persistent anxiety
- Cold, clammy skin
Some factors raise your chances of getting pulmonary edema. These include high blood pressure, diabetes, heart disease, and obesity6.
If you have sudden, severe breathing problems, get emergency help fast. Don’t wait if you see blood-tinged frothy sputum.
“Early recognition of symptoms can be life-saving in pulmonary edema cases.” – Medical Respiratory Experts
You might also feel very tired, have swollen legs, or a worsening cough. Listen to your body and call a doctor if something feels wrong.
Pulmonary edema can quickly become deadly5. Acting fast and knowing the signs can help manage this serious breathing problem.
Treatment Options and Emergency Care for Pulmonary Edema
Fast medical help is crucial when pulmonary edema strikes. Your knowledge of treatment methods can be life-saving. Understanding this serious condition can make a real difference.
Immediate Medical Interventions
Emergency care for pulmonary edema aims to stabilize breathing and reduce fluid buildup. Doctors will focus on giving oxygen and quickly assessing your condition.
Medical professionals prioritize rapid assessment to ensure proper treatment. Their main goal is to help you breathe better and feel more comfortable.
- Oxygen therapy targeting 92-96% saturation7
- Non-invasive ventilation for respiratory distress7
- Rapid cardiovascular monitoring
Medication and Oxygen Therapy
Treatment for pulmonary edema involves careful medication management. The approach depends on whether you have cardiogenic or noncardiogenic edema. Your doctor will choose the best medicines for your specific condition.
| Medication Type | Primary Function |
|---|---|
| Diuretics | Reduce fluid retention |
| ACE Inhibitors | Improve cardiovascular function |
| Inotropic Agents | Support heart muscle performance |
Long-term Management Strategies
Managing pulmonary edema requires more than just immediate treatment. Your long-term plan should include lifestyle changes and regular doctor visits. This approach helps prevent future episodes and improves overall health.
- Regular cardiovascular check-ups
- Maintaining a heart-healthy diet
- Managing underlying health conditions
- Following prescribed medication regimens
Effective pulmonary edema management demands proactive healthcare engagement and personalized treatment plans.
Remember, early detection and prompt treatment significantly improve your chances of recovery7.
Conclusion
Pulmonary edema is a serious respiratory condition. It can develop quickly, causing breathing problems and low oxygen levels. Early detection and prompt medical care are vital for recovery. Medical research supports early detection8.
Your proactive approach can make a big difference. Regular check-ups and managing heart conditions help prevent pulmonary edema. Some activities, like high-altitude trekking, carry specific risks9. Being aware of these risks helps you make safer health choices.
Managing pulmonary edema requires a thorough plan. This includes medical monitoring, targeted treatments, and lifestyle changes. Many people successfully manage this condition with proper care and commitment8.
Stay informed and keep talking with your doctors. Listen to your body’s signals. Your awareness and quick action are key to managing this complex respiratory condition.
FAQ
What is pulmonary edema?
What are the main types of pulmonary edema?
What are the key symptoms of pulmonary edema?
How is high-altitude pulmonary edema (HAPE) different?
What are the emergency treatments for pulmonary edema?
What are the risk factors for developing pulmonary edema?
Can pulmonary edema be prevented?
When should I seek immediate medical attention?
Source Links
- Pulmonary edema-Pulmonary edema – Symptoms & causes – Mayo Clinic – https://www.mayoclinic.org/diseases-conditions/pulmonary-edema/symptoms-causes/syc-20377009
- Pulmonary Edema: Symptoms, Causes, and Treatment – https://www.healthline.com/health/pulmonary-edema
- Pulmonary Edema – StatPearls – NCBI Bookshelf – https://www.ncbi.nlm.nih.gov/books/NBK557611/
- Pulmonary edema – https://www.beaconhealthsystem.org/library/diseases-and-conditions/pulmonary-edema?content_id=CON-20376993
- Pulmonary edema – UF Health – https://ufhealth.org/conditions-and-treatments/pulmonary-edema
- Pulmonary edema – https://www.mountsinai.org/health-library/condition/pulmonary-edema
- Managing acute pulmonary oedema – PMC – https://pmc.ncbi.nlm.nih.gov/articles/PMC5408000/
- Unilateral pulmonary edema: a case report and review of the literature – Journal of Medical Case Reports – https://jmedicalcasereports.biomedcentral.com/articles/10.1186/s13256-018-1739-3
- Frontiers | An update on environment-induced pulmonary edema – “When the lungs leak under water and in thin air” – https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2022.1007316/full