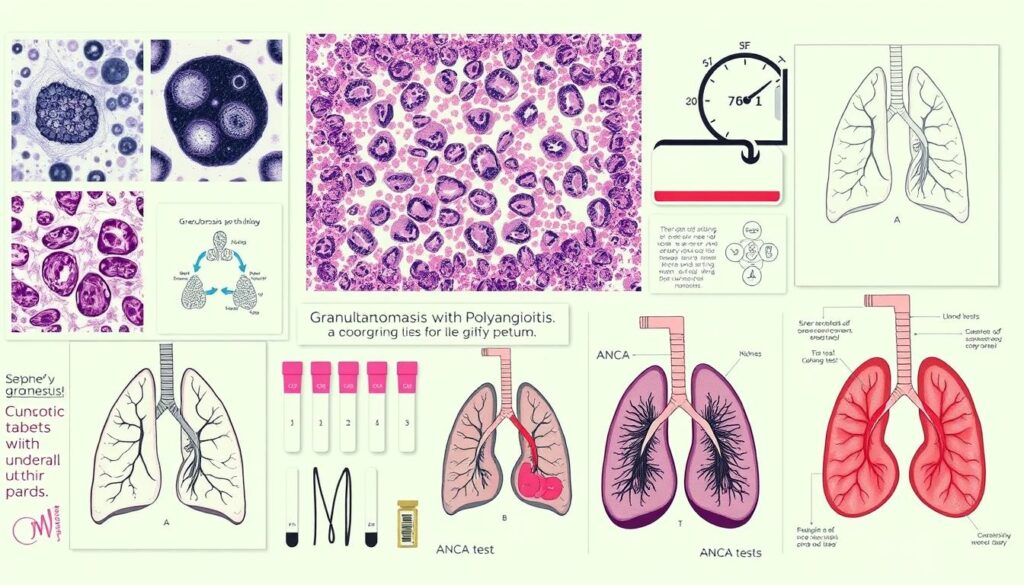
Granulomatosis with Polyangiitis (GPA) is a rare autoimmune disorder that causes blood vessel inflammation. It’s a serious condition that affects your respiratory system and kidneys. GPA can impact multiple organs if left untreated.
Without proper care, GPA may lead to severe complications. These include pulmonary hemorrhage, kidney failure, and vision loss. Early diagnosis is key for effective management of this disorder.
Medical research has made great progress in treating GPA. In 2021, the FDA approved Avacopan (Tavneos®) for severe ANCA-associated vasculitis. This new treatment offers hope to patients struggling with GPA1.
Key Takeaways
- GPA is a rare autoimmune disorder causing blood vessel inflammation
- Respiratory system and kidneys are primary targets of the disease
- Early diagnosis is critical for effective management
- Multiple treatment options are available
- Ongoing medical research continues to improve treatment strategies
What is Granulomatosis with Polyangiitis
Granulomatosis with polyangiitis (GPA) is a rare autoimmune disorder affecting multiple body systems. It causes inflammation in small and medium-sized blood vessels. This can lead to damage in various organs2.
Understanding ANCA-Associated Vasculitis
Anti-Neutrophil Cytoplasmic Antibody (ANCA) is key in this autoimmune disorder. It triggers inflammatory responses that can harm tissues. In ANCA-associated vasculitis, antibodies mistakenly attack healthy cells3.
Who is at Risk for GPA
GPA can affect people of any age. However, it’s most common in adults between 40 and 65 years old3.
Risk factors include:
- Age range of 40-65 years
- Potential genetic predispositions
- Possible environmental triggers
- Weakened immune system
Role of Anti-Neutrophil Cytoplasmic Antibodies
Proteinase 3 ANCA is a specific antibody linked to GPA development. These antibodies can cause inflammation by attacking neutrophils. This can potentially lead to organ damage4.
“Understanding the complex interactions of ANCA is crucial for managing this challenging autoimmune condition.”
Early detection is vital for managing Granulomatosis with Polyangiitis. Comprehensive medical monitoring is also essential for effective treatment.
Common Signs and Manifestations of Respiratory and Kidney Involvement
GPA impacts multiple organ systems with complex symptoms. Early detection helps patients get timely medical care. This prevents serious complications and improves outcomes.
Early Warning Signs and Symptoms
GPA’s early stages often look like common respiratory infections. You might have persistent sinus inflammation that doesn’t improve with usual treatments.
Key early signs include frequent nosebleeds, nasal congestion, and sinus pain. Chronic ear infections, unexplained fever, and fatigue are also common.
- Frequent nosebleeds
- Nasal congestion
- Sinus pain and pressure
- Chronic ear infections
- Unexplained fever and fatigue
Organ-Specific Manifestations
Respiratory symptoms can worsen quickly, causing serious issues. GPA may trigger lung inflammation, leading to bloody coughs and breathing difficulties5.
Kidney problems might start subtly. Look for changes in urine color or unexpected swelling6.
Critical Complications to Watch For
Without proper care, GPA can severely damage organs. Be aware of these potential critical complications:
- Lung hemorrhage
- Rapidly progressive kidney disease
- Permanent damage to eyes and ears
Early diagnosis and comprehensive treatment are crucial for managing GPA effectively6.
Blood and urine tests help detect kidney issues and track the disease. Patients should team up with their doctors to create a tailored treatment plan6.
Treatment Options and Management Strategies
GPA treatment depends on disease severity and organ involvement. This complex autoimmune disorder requires a tailored approach7.
- Induction Phase: Targeting active inflammation
- Maintenance Phase: Preventing disease relapse
Milder cases often use a mix of medications. Doctors pair glucocorticoids like prednisone with methotrexate to manage ANCA-associated vasculitis8.
| Treatment Phase | Recommended Medications | Key Considerations |
|---|---|---|
| Induction | Rituximab, Cyclophosphamide | High-dose therapy to control inflammation |
| Maintenance | Azathioprine, Methotrexate | Prevent disease recurrence |
Severe cases need stronger treatments. Doctors use biologic drugs like rituximab or cyclophosphamide with glucocorticoids. In 2021, avacopan (Tavneos®) became a new option for severe ANCA-associated vasculitis7.
“Personalized treatment is crucial in managing this complex autoimmune condition.” – Vasculitis Research Team
Kidney complications may require dialysis or transplantation. Plasmapheresis helps in extreme cases affecting kidneys or lungs8.
Your doctor will create a plan based on your symptoms and health. Regular check-ups and medication adjustments are key to managing this condition effectively.
Conclusion
Living with Granulomatosis with Polyangiitis (GPA) can be challenging. This rare autoimmune disorder affects about 12 in a million people yearly9. Early detection and proper treatment are vital for managing GPA10.
Medical progress has greatly improved patient outcomes. With the right care, you can achieve remission and live well. Studies show that combining steroids and immunosuppressants can lead to remission in 75%-90% of GPA patients11.
Your treatment plan may include careful monitoring. Advanced diagnostic techniques help doctors track your progress9. Remember, you’re not alone in facing GPA.
About 90% of patients have ANCA-positive antibodies, allowing for targeted treatments11. Regular check-ups and following your treatment plan are crucial. Your active role can greatly impact your health and well-being10.
FAQ
What is Granulomatosis with Polyangiitis (GPA)?
Who is most likely to develop GPA?
What are the early symptoms of GPA?
How is GPA diagnosed?
What are the primary treatment options for GPA?
Can GPA be cured?
What organs can GPA affect?
What are the potential complications of untreated GPA?
Is GPA a hereditary condition?
How often do patients with GPA experience remission and relapse?
Source Links
- Granulomatosis with Polyangiitis – https://vasculitisfoundation.org/education/vasculitis-types/granulomatosis-with-polyangiitis/
- Granulomatosis with polyangiitis (GPA) – https://www.nhs.uk/conditions/granulomatosis-with-polyangiitis/
- Granulomatosis with Polyangiitis – https://www.hopkinsmedicine.org/health/conditions-and-diseases/wegeners-granulomatosis
- Granulomatosis with Polyangiitis (GPA, formerly Wegener Granulomatosis): Practice Essentials, Background, Etiology – https://emedicine.medscape.com/article/332622-overview
- Granulomatosis with polyangiitis – https://www.mountsinai.org/health-library/diseases-conditions/granulomatosis-with-polyangiitis
- Granulomatosis with polyangiitis – Symptoms and causes – https://www.mayoclinic.org/diseases-conditions/granulomatosis-with-polyangiitis/symptoms-causes/syc-20351088
- Current therapy of granulomatosis with polyangiitis and microscopic polyangiitis: the role of rituximab – https://pmc.ncbi.nlm.nih.gov/articles/PMC4322237/
- EULAR recommendations for the management of ANCA-associated vasculitis: 2022 update – https://ard.bmj.com/content/83/1/30
- A challenging case of granulomatosis with polyangiitis with cardiac involvement: a rare case report – https://acr.amegroups.org/article/view/7321/html
- Granulomatosis with polyangiitis: clinical characteristics and updates in diagnosis – https://pmc.ncbi.nlm.nih.gov/articles/PMC11385631/
- Granulomatosis With Polyangiitis: The Complexity of Clinical Manifestations, Therapeutic Challenges, and Complications of a Severe Multisystemic Case – https://pmc.ncbi.nlm.nih.gov/articles/PMC10642917/