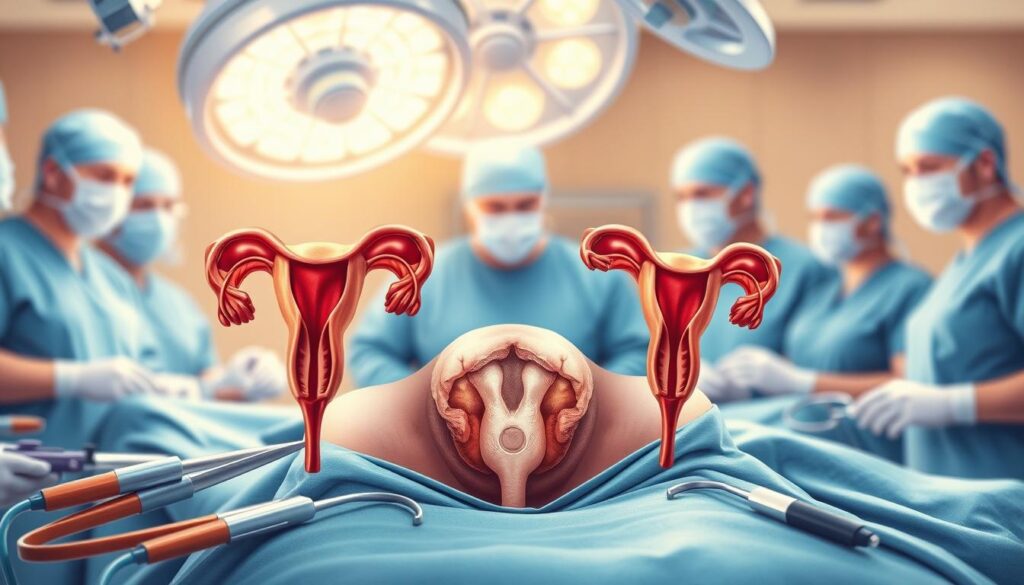
Oophorectomy is a crucial surgery that removes one or both ovaries. It addresses various women’s health issues, including ovarian cancer prevention and complex reproductive conditions1.
This surgery can be a vital part of your reproductive health journey. Different surgical approaches are available, based on your specific medical needs2.
Oophorectomy may be necessary for women at risk of ovarian cancer. The general population has a one in 80 chance of developing this cancer1.
Key Takeaways
- Oophorectomy is a surgical procedure to remove one or both ovaries
- Multiple surgical approaches exist for ovary removal
- The procedure can help manage various reproductive health conditions
- Potential risks and recovery processes vary by individual
- Consultation with a healthcare professional is crucial before deciding on surgery
What is Oophorectomy: Types and Medical Purpose
Oophorectomy is a surgery to remove one or both ovaries. This procedure can significantly impact your reproductive health. Learning about it helps in making informed medical choices3.
Defining Surgical Approaches
Oophorectomy can be performed in two primary ways:
- Unilateral oophorectomy: Removal of a single ovary
- Bilateral oophorectomy: Removal of both ovaries
The surgery typically lasts about 30 minutes. It requires specialized techniques for successful completion4.
Common Medical Indications
Doctors may recommend oophorectomy for various medical conditions:
- Treating ovarian cancer
- Managing severe endometriosis
- Removing persistent ovarian cysts
- Reducing cancer risk in high-risk patients
Surgical Considerations and Combinations
Oophorectomy might be combined with a hysterectomy in some cases. For patients with BRCA mutations, doctors may suggest a risk-reducing bilateral salpingo-oophorectomy3.
Your healthcare provider will help determine the most appropriate surgical approach based on your individual medical needs.
| Procedure Type | Potential Impacts |
|---|---|
| Unilateral Oophorectomy | Minimal fertility impact if remaining ovary is healthy |
| Bilateral Oophorectomy | Immediate menopause and potential long-term health considerations |
Careful thought is vital, especially for younger patients. Preserving ovarian function can be crucial for long-term health3.
Surgical Approaches and Recovery Process
Oophorectomy offers multiple surgical approaches. Each method impacts your recovery differently. The main options are laparoscopic, traditional laparotomy, and robotic surgery5.
Laparoscopic surgery is a minimally invasive technique. It uses smaller incisions and results in less pain. Patients often recover faster than with traditional open surgery5.
This approach offers several benefits. These include shorter hospital stays and minimal scarring. Patients also face a lower risk of complications.
- Shorter hospital stays
- Minimal scarring
- Reduced risk of complications
- Quicker return to normal activities
Recovery time varies based on the surgical method used. Your individual health also plays a role. Most patients can resume full activity within 2 to 4 weeks6.
“Choosing the right surgical approach is crucial for optimal recovery and minimizing potential risks.” – Medical Experts
Oophorectomy carries some risks. These include bleeding, infection, and possible damage to nearby organs5. Your doctor will guide you through post-surgery care.
Post-surgical care may involve several steps. These can include managing medications and limiting heavy lifting. You’ll also need to care for your incision carefully.
- Medication management
- Restriction on heavy lifting
- Careful incision care
- Monitoring for potential complications
Note: Consult with your healthcare professional to determine the most appropriate surgical approach for your specific medical needs.
Conclusion
Understanding the long-term effects of oophorectomy is vital for your health. This surgery requires careful consideration of risks and benefits. Bilateral salpingo-oophorectomy rates vary with age, from 19% in women under 45 to 81% over 557.
Fertility preservation is crucial for younger women considering this surgery. Women under 45 should be extra cautious due to potential health impacts8. Surgical menopause can affect your quality of life through complex hormonal changes.
Hormone replacement therapy may help manage these transitions, especially after early ovarian removal. The long-term effects of oophorectomy differ across age groups. Research shows possible risks of cardiovascular and neurological changes8.
Your healthcare provider can guide you through potential outcomes. They’ll help you make an informed decision aligned with your health goals. Your oophorectomy journey is unique to you.
Open communication with doctors is essential. Understanding risks and personalizing hormone management are key to optimal health outcomes. Your decision should fit your specific medical needs, age, and long-term health objectives.
FAQ
What is an oophorectomy?
What are the different types of oophorectomy?
Why might I need an oophorectomy?
How is an oophorectomy performed?
What happens to my hormones after an oophorectomy?
Will an oophorectomy affect my fertility?
What are the potential risks of the surgery?
How long is the recovery process?
Can I prevent the need for an oophorectomy?
Source Links
- Oophorectomy: Indications, Procedure, and Risks – https://drseckin.com/oophorectomy-indications-procedure-and-risks/
- Learning About Oophorectomy | Kaiser Permanente – https://healthy.kaiserpermanente.org/health-wellness/health-encyclopedia/he.learning-about-oophorectomy.abn2046
- Oophorectomy – StatPearls – NCBI Bookshelf – https://www.ncbi.nlm.nih.gov/books/NBK559235/
- Laparoscopic oophorectomy – https://www.healthdirect.gov.au/surgery/laparoscopic-oophorectomy
- Surgical Procedures: Oophorectomy | OncoLink – https://www.oncolink.org/cancers/gynecologic/treatments/surgical-procedures-oophorectomy
- Oophorectomy (ovary removal surgery) – Mayo Clinic – https://www.mayoclinic.org/tests-procedures/oophorectomy/about/pac-20385030
- Association of bilateral salpingo-oophorectomy with all cause and cause specific mortality: population based cohort study – https://www.bmj.com/content/375/bmj-2021-067528
- Salpingo-oophorectomy at the Time of Benign Hysterectomy: A Systematic Review – https://scholars.uthscsa.edu/en/publications/salpingo-oophorectomy-at-the-time-of-benign-hysterectomy-a-system