Low blood pressure can surprise you when standing up quickly. Orthostatic hypotension causes sudden dizziness and fainting when rising from sitting. This condition affects many older adults, creating unexpected daily challenges12.
Imagine feeling dizzy every time you get up. For seniors, this is a common health issue. About 18% of people 65 or older face this problem in the U.S12.
Shockingly, orthostatic hypotension accounts for 35% of elderly hospital admissions1. This condition disrupts the body’s normal blood pressure adjustment when standing.
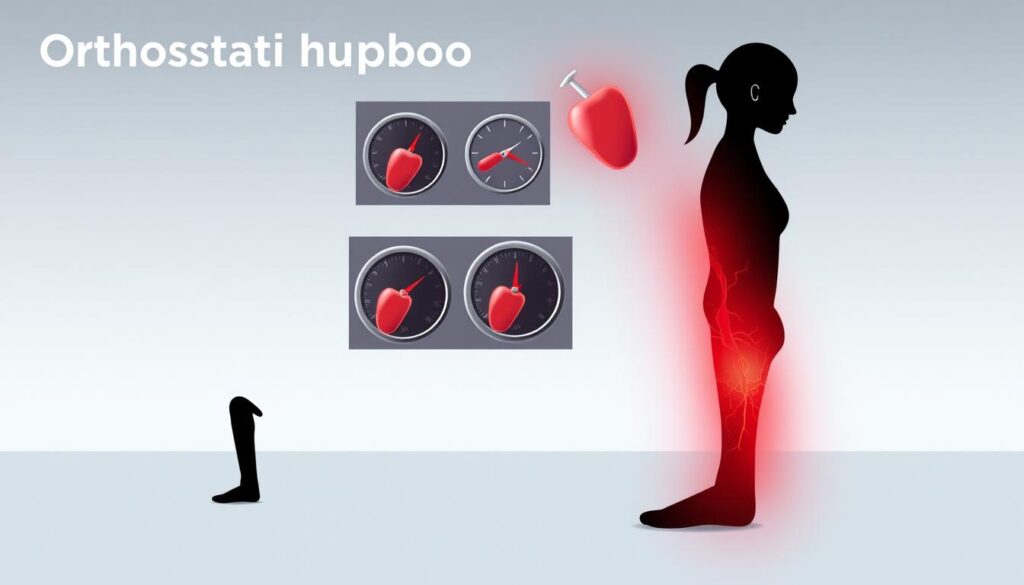
Patients often experience a blood pressure drop of 20/10 mmHg within three minutes of standing1. Many people don’t know they have it. Up to two-thirds of cases go unnoticed without proper medical checks2.
Key Takeaways
- Orthostatic hypotension affects nearly 18% of adults over 65
- Sudden dizziness can occur when changing body positions
- Blood pressure drops significantly within minutes of standing
- Many cases remain undiagnosed without specific testing
- Elderly individuals are most vulnerable to this condition
What is Orthostatic Hypotension and Its Impact on Daily Life
Orthostatic hypotension disrupts daily activities by affecting blood flow when changing positions. This blood pressure disorder makes standing up challenging. Understanding it helps manage potential health risks effectively.
Common Symptoms and Warning Signs
Recognizing orthostatic hypotension symptoms is crucial for early intervention. Common signs include lightheadedness and dizziness when standing or changing positions.
Other symptoms are fainting episodes, blurred vision, and feeling weak or unsteady. These occur when blood pressure drops suddenly due to various triggers3.
- Lightheadedness upon standing
- Dizziness after changing positions
- Potential fainting episodes
- Blurred vision
- Weakness or feeling unsteady
Fainting is a serious symptom that needs immediate attention. It can happen when blood pressure drops too low.
Risk Factors and Vulnerable Groups
Some groups are more likely to develop orthostatic hypotension. Elderly health is especially affected, with people over 65 at higher risk4.
Key risk factors include advanced age, certain medications, and underlying health conditions. Prolonged bed rest and dehydration also increase the chances.
- Advanced age
- Certain medications
- Underlying health conditions
- Prolonged bed rest
- Dehydration
“Approximately one in five older adults experiences orthostatic hypotension, making it a significant health concern.”
How Blood Pressure Changes Affect Your Body
Autonomic dysfunction is central to orthostatic hypotension. When the body can’t regulate blood pressure well, it leads to potential problems.
These issues may include falls, reduced mobility, and increased cardiovascular risks5. Understanding these effects helps you take steps to manage your health.
Diagnosing and Measuring Blood Pressure Changes
Blood Pressure Monitoring is crucial for diagnosing orthostatic hypotension. Healthcare providers use specialized tests to assess your body’s blood pressure response. These tests help accurately measure changes in your blood pressure.
Orthostatic hypotension occurs when blood pressure drops significantly upon changing positions. It’s defined by a 20 mmHg drop in systolic pressure or 10 mmHg in diastolic pressure. This change must happen within 3 minutes of standing6.
Medical Tests and Evaluations
Several key medical tests help diagnose orthostatic hypotension:
- Electrocardiogram (ECG) to assess heart electrical activity
- Tilt Table Test to evaluate blood pressure changes
- Blood tests to rule out underlying conditions
- Ambulatory blood pressure monitoring
Orthostatic hypotension affects 5-16% of middle-aged adults. In elderly care facilities, it impacts over 50% of patients6.
Understanding Blood Pressure Numbers
| Measurement Type | Normal Range | Potential Concern |
|---|---|---|
| Systolic Pressure | Less than 120 mmHg | Drop of 20 mmHg or more |
| Diastolic Pressure | Less than 80 mmHg | Drop of 10 mmHg or more |
When to Seek Medical Help
Contact a healthcare professional if you have persistent symptoms like:
- Frequent dizziness
- Lightheadedness when standing
- Blurred vision
- Unexplained fainting episodes
Early detection and proper diagnosis can significantly improve management of orthostatic hypotension6.
Continuous Blood Pressure Monitoring offers more accurate diagnostic insights than interval measurements7. Your doctor will choose the best testing method for your situation. This approach ensures a thorough evaluation of your blood pressure changes.
Essential Management Strategies for Low Blood Pressure
Managing orthostatic hypotension requires a mix of lifestyle changes and medical help. Your doctor can create a plan to address low blood pressure. This approach aims to boost your quality of life8.
Compression stockings are key in managing blood flow and easing symptoms. These special garments stop blood from pooling in your legs. They can greatly improve your overall circulation8.
For best results, choose waist-high compression stockings. They offer maximum effectiveness in managing blood flow.
- Stay hydrated by drinking plenty of water throughout the day
- Monitor your salt intake under medical supervision
- Avoid excessive alcohol consumption
- Practice slow position changes to prevent sudden blood pressure drops
Some medications can cause orthostatic hypotension. Your doctor might adjust your current meds or prescribe new ones. Drugs like midodrine, droxidopa, or fludrocortisone can help stabilize blood pressure8.
*Small, strategic changes can make a big difference in managing low blood pressure.*
Lifestyle changes play a crucial role in managing this condition. Eating small, low-carb meals can help reduce symptoms. Regular exercise is also beneficial9.
Pay attention to how your body reacts to different activities and positions. This awareness can help you better manage your condition.
Track your symptoms and blood pressure readings regularly. Use the comprehensive monitoring approach recommended by medical experts. This data will help you and your doctor create an effective management plan8.
Conclusion
Managing blood pressure requires a comprehensive approach. Older adults are more likely to experience orthostatic hypotension. Understanding your health profile can help develop an effective Blood Pressure Management strategy.
Regular monitoring and proactive healthcare engagement are essential. Track your symptoms and work closely with medical professionals. clinical research provides valuable insights into treating neurogenic orthostatic hypotension10.
Fall prevention is crucial. Studies show that orthostatic symptoms can increase fall risk significantly11. Personalized treatment is key to managing this condition effectively.
Intensive blood-pressure treatments have shown promising results in reducing cardiovascular risks10. Your doctor can design a tailored plan addressing your specific needs. This may include lifestyle changes, medication adjustments, and targeted interventions.
Stay informed and maintain open communication with your healthcare team. Follow recommended guidelines to manage neurogenic orthostatic hypotension successfully. You can maintain an active, fulfilling lifestyle with proper care.
FAQ
What exactly is orthostatic hypotension?
Who is most at risk for developing orthostatic hypotension?
How is orthostatic hypotension diagnosed?
What are the most effective ways to manage orthostatic hypotension?
Can orthostatic hypotension be completely cured?
What should I do if I feel dizzy when standing up?
Are there any long-term complications of orthostatic hypotension?
Source Links
- Orthostatic hypotension: Causes, symptoms, and prevention – https://www.medicalnewstoday.com/articles/318158
- Evaluation and Management of Orthostatic Hypotension – https://www.aafp.org/pubs/afp/issues/2011/0901/p527.html
- Orthostatic hypotension (postural hypotension)-Orthostatic hypotension (postural hypotension) – Symptoms & causes – Mayo Clinic – https://www.mayoclinic.org/diseases-conditions/orthostatic-hypotension/symptoms-causes/syc-20352548
- The Prevalence of Orthostatic Hypotension: A Systematic Review and Meta-Analysis – https://pmc.ncbi.nlm.nih.gov/articles/PMC6909901/
- Postural Hypotension (Orthostatic Hypotension): What to Know – https://www.verywellhealth.com/postural-hypotension-7974812
- Orthostatic hypotension – a practical approach to investigation and management – https://pmc.ncbi.nlm.nih.gov/articles/PMC5693784/
- Diagnosing orthostatic hypotension with continuous and interval blood pressure measurement devices – Journal of Human Hypertension – https://www.nature.com/articles/s41371-018-0091-9
- Low blood pressure (hypotension) – Diagnosis and treatment – https://www.mayoclinic.org/diseases-conditions/low-blood-pressure/diagnosis-treatment/drc-20355470
- Orthostatic Hypotension: A Practical Approach – https://www.aafp.org/pubs/afp/issues/2022/0100/p39.html
- New Study Shows Intensive Blood-Pressure Treatment Effective Regardless of Hypotension – https://www.marcusinstituteforaging.org/news/new-study-shows-intensive-blood-pressure-treatment-effective-regardless-hypotension
- Timing of orthostatic hypotension and its relationship with falls in older adults – https://pure.johnshopkins.edu/en/publications/timing-of-orthostatic-hypotension-and-its-relationship-with-falls