Acquired third nerve palsy can drastically affect your eye’s movement and function. This condition impacts the oculomotor nerve, which controls important eye movements and eyelid positioning1. It can significantly alter your vision and daily activities2.
This eye disorder is fairly uncommon, with about 4 cases per 100,000 people each year1. Your risk goes up as you age, especially after 601.
The most frequent causes include microvascular problems, trauma, and possible neurological compressions3.
Key Takeaways
- Third nerve palsy impacts eye movement and function
- Prevalence increases with age, especially after 60
- Multiple potential causes exist, from microvascular to traumatic
- Proper diagnosis requires comprehensive neurological assessment
- Early recognition can improve treatment outcomes
Understanding Acquired 3rd Nerve Palsy
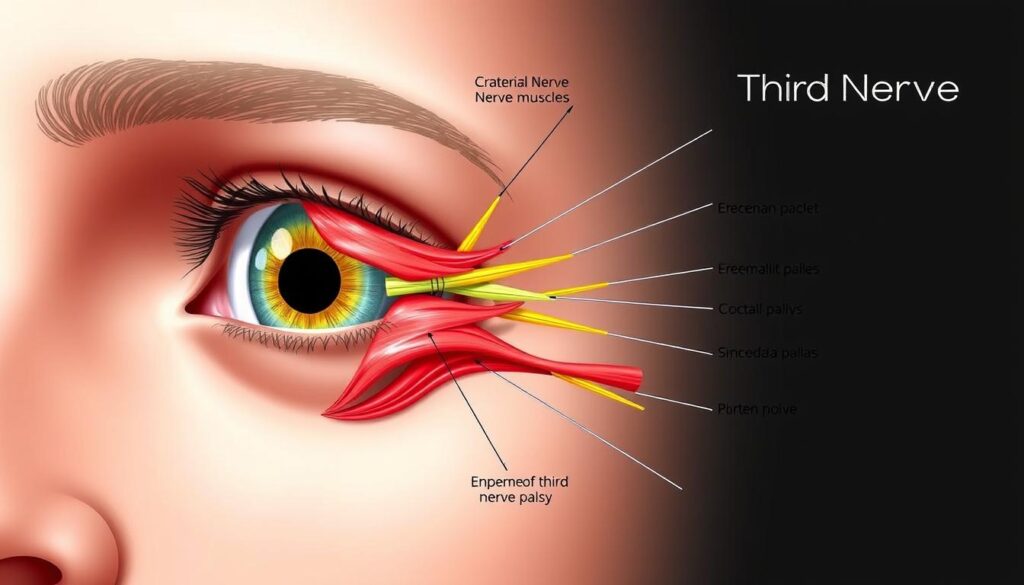
The oculomotor nerve is vital for eye movement and function. When disrupted, it can greatly affect your vision and daily activities4.
Clinical Definition and Anatomy
Your oculomotor nerve has a complex structure. It controls four of the six extraocular muscles. These include the superior, inferior, and medial recti, plus the inferior oblique muscle4.
This nerve also manages other important functions. These include the levator muscle of the eyelid, pupillary function, and eye movement coordination.
- Levator muscle of the eyelid
- Pupillary function
- Eye movement coordination
Common Manifestations
Third nerve palsy can show up in different ways. It can range from partial to complete disruption. The symptoms depend on where the nerve is damaged4.
| Nerve Fiber Type | Potential Symptoms |
|---|---|
| Outer Nerve Fibers | Muscle and pupil constriction issues5 |
| Inner Nerve Fibers | Eye misalignment, impaired lid elevation5 |
Impact on Vision and Daily Life
Affected extraocular muscles can cause challenging symptoms. These may include diplopia (double vision) and problems with depth perception5. Young patients might not always express these visual changes clearly.
Professional assessment is crucial for accurate diagnosis. Early detection and thorough evaluation are key to managing this condition effectively.
Early detection and comprehensive evaluation are key to managing third nerve palsy effectively.
Several conditions can trigger third nerve palsy. These include diabetes, high blood pressure, and inflammatory diseases5. In children, up to half of the cases might be present at birth5.
Causes and Risk Factors of Oculomotor Nerve Palsy
Knowing the causes of oculomotor nerve palsy is vital for proper care. Many factors can lead to this neurological condition. Microvascular ischemia is the most common cause6.
Diabetes and high blood pressure are key factors in nerve palsy. About 18% of oculomotor palsy cases link to diabetes mellitus7.
Risk increases with age, particularly after 50 years old.
Age-specific insights reveal interesting patterns:
| Age Group | Microvascular Ischemia Prevalence |
|---|---|
| Under 50 years | 49% of cases6 |
| 50 years and older | 83% of cases6 |
Additional risk factors include:
- Smoking
- Previous stroke
- Coronary artery disease
- Dyslipidemia6
Some cases remain idiopathic, or without a known cause. Knowing these risk factors helps catch and manage oculomotor nerve palsy early8.
Diagnosis and Clinical Presentation
Third nerve palsy diagnosis requires a thorough approach. It combines careful clinical examination and advanced diagnostic techniques. Your doctor will evaluate the underlying cause and potential implications of this condition.
Physical Examination Methods
Your doctor will assess eye movement to identify neurological changes. They’ll focus on key areas during the examination.
- Evaluating pupil involvement9
- Checking eye alignment and movement
- Assessing eyelid position
- Documenting any visual disturbances
Diagnostic Procedures and Neuroimaging
Neuroimaging is crucial in diagnosing third nerve palsy. Specialists recommend prompt imaging to identify potential underlying causes.
CT and CTA are preferred for adults with arteriosclerotic risk factors10.
| Imaging Technique | Primary Use |
|---|---|
| CT Angiography | Identifying aneurysms in adults |
| MRI | Detecting soft tissue abnormalities |
Distinguishing Features and Signs
The clinical presentation varies significantly with age. For individuals over 60, the annual incidence of isolated third nerve palsy is 12.5 per 100,000.
This compares to just 1.7 per 100,000 in younger populations9. Microvascular ischemia is often the primary cause in older patients11.
Pupil involvement can be a critical diagnostic indicator, often signaling a potential compressive lesion that requires immediate attention.
These detailed diagnostic approaches help ensure accurate identification of third nerve palsy. They also guide appropriate treatment for this condition.
Conclusion
Managing acquired 3rd nerve palsy requires a tailored approach. Research shows patients have a promising outlook for recovery. The overall recovery rate of 85.2% offers hope.
Treatment options depend on the underlying cause. Microvascular issues are common in patients over 50 years old6. Early medical attention and managing treatable conditions increase chances of complete recovery12.
Healthcare teams may suggest occlusion therapy for diplopia. Surgical interventions might be considered for persistent cases. A multidisciplinary approach and regular follow-ups are crucial for successful treatment.
Some patients achieve full recovery within 3.5 months. Others may experience residual deficits12. Your treatment plan will be designed to maximize recovery potential.
FAQ
What is acquired 3rd nerve palsy?
What are the most common causes of 3rd nerve palsy?
How is 3rd nerve palsy diagnosed?
What are the symptoms of 3rd nerve palsy?
Who is at higher risk for developing 3rd nerve palsy?
Can 3rd nerve palsy be treated?
What is the prognosis for 3rd nerve palsy?
How does 3rd nerve palsy affect eye movement?
Source Links
- The causes of acquired 3rd nerve palsy – https://www.mayoclinic.org/medical-professionals/ophthalmology/news/the-causes-of-acquired-third-nerve-palsy/mac-20431238
- Acquired Oculomotor Nerve Palsy – EyeWiki – https://eyewiki.org/Acquired_Oculomotor_Nerve_Palsy
- Incidence and Etiologies of Acquired Third Nerve Palsy Using a Population-Based Method – https://pmc.ncbi.nlm.nih.gov/articles/PMC5462106/
- Third cranial nerve (oculomotor nerve) palsy in adults – https://www.uptodate.com/contents/third-cranial-nerve-oculomotor-nerve-palsy-in-adults
- No title found – https://www.allaboutvision.com/conditions/related/third-nerve-palsy/
- Acquired Ocular Motor Nerve Palsy in Neurology Clinics: A Prospective Multicenter Study – https://www.thejcn.com/DOIx.php?id=10.3988/jcn.2019.15.2.221
- Isolated Third Cranial Nerve Palsy: Aetiology – Clinical Profile and Recovery at a Tertiary Neuro-ophthalmology Centre on the East Coast Peninsular of Malaysia | Nurul-Ain – https://www.jhsmr.org/index.php/jhsmr/article/view/901
- Third Nerve Palsy – American Association for Pediatric Ophthalmology and Strabismus – https://aapos.org/glossary/third-nerve-palsy
- Isolated third nerve palsy: Lessons from the literature and 4 case studies – https://www.mdedge9-ma1.mdedge.com/familymedicine/article/261713/mixed-topics/isolated-third-nerve-palsy-lessons-literature-and-4-case
- Third nerve palsy | MedLink Neurology – https://www.medlink.com/articles/third-nerve-palsy
- Self-Resolving Ischemic Third Nerve Palsy – https://webeye.ophth.uiowa.edu/eyeforum/cases/280-self-resolving-ischemic-TNP.htm
- Clinical features and natural history of acquired third, fourth, and sixth cranial nerve palsy – Eye – https://www.nature.com/articles/6702720