Bursitis is a painful joint condition affecting small fluid-filled sacs called bursae. These sacs cushion bones, tendons, and muscles near joints. Bursitis commonly impacts shoulder, elbow, and hip joints1.
Your bursitis risk increases with age and certain lifestyle factors. Repetitive motions or prolonged pressure can trigger bursa swelling. Carpet laying, gardening, and playing musical instruments can heighten tendon pain chances1.
Medical conditions like rheumatoid arthritis, gout, and diabetes contribute to bursitis development1. Excess weight can increase hip and knee bursitis risk1. Recurrent flare-ups are common, indicating potential chronic issues despite treatment1.
Understanding causes and risk factors helps protect your joint health. Take proactive steps to prevent bursitis and maintain overall well-being.
Key Takeaways
- Bursitis affects fluid-filled sacs near joints
- Shoulder, elbow, and hip joints are most vulnerable
- Repetitive motions can trigger joint inflammation
- Certain medical conditions increase bursitis risk
- Prevention involves maintaining a healthy weight and proper exercise
Understanding Bursitis and Its Impact on Joint Health
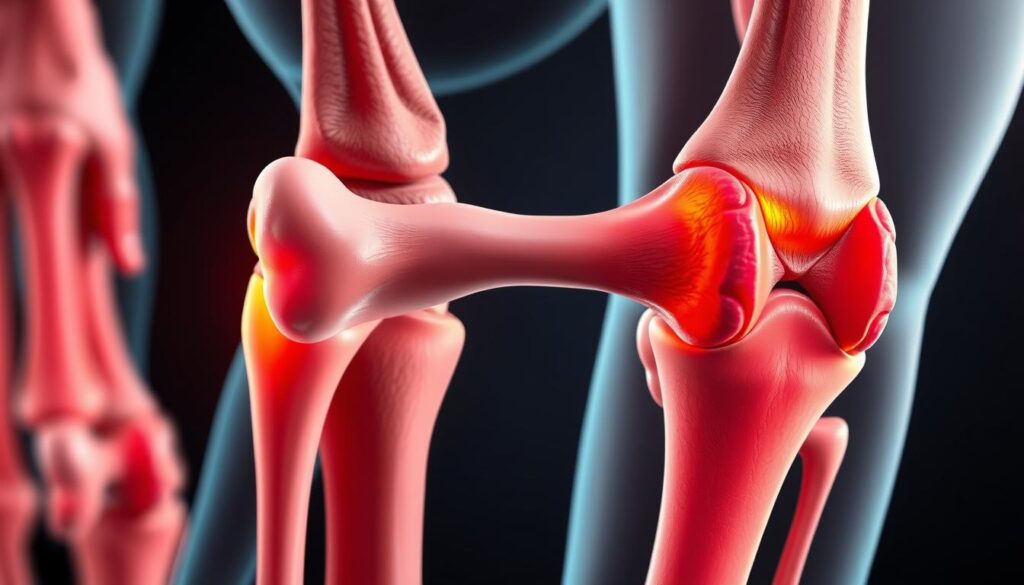
Bursitis affects many people’s mobility and comfort. Your body has small fluid-filled sacs called bursae. These cushions reduce friction between tissues and joints2.
Bursae help your body move smoothly. They protect against repetitive strain injuries3. When inflamed, they can cause discomfort and limit motion.
What Are Bursae and Their Function
Bursae are natural shock absorbers in your body. They prevent tissues from rubbing directly against each other. Inflamed bursae can cause significant discomfort2.
Simple movements can become painful experiences. Your range of motion may be limited due to this inflammation.
Common Locations of Bursitis
Bursitis can impact multiple areas of your body, including:
- Shoulder
- Elbow
- Hip
- Knees
- Buttocks
- Calf
Athletes, manual laborers, and musicians are at risk. Their repetitive movements make them prone to this rheumatic disorder3.
Risk Factors and Contributing Conditions
Several factors can increase your chances of developing bursitis:
- Repetitive motion activities
- Age-related changes
- Sports injuries
- Underlying health conditions like diabetes
- Inflammatory diseases
Overuse injuries can trigger bursitis. This causes swelling, tenderness, and limited joint movement3. Most cases are acute and can heal with proper treatment4.
Understanding your body’s signals is key to preventing and managing bursitis effectively.
Recognizing Symptoms and Treatment Options
Bursitis can greatly affect your joint health. It shows up as joint pain, swelling, and redness. Your body has over 150 potential bursae, with common spots in the elbow, knee, and shoulder56.
Spotting symptoms early helps you get the right treatment. Watch out for these signs:
- Persistent joint pain during movement
- Localized swelling and tenderness
- Redness around the affected joint
- Reduced range of motion
Different types of bursitis have unique symptoms. Chronic bursitis grows slowly from repeated irritation6.
Infected bursitis needs quick medical care. It causes extreme warmth, pain, and possible fever6.
| Bursitis Type | Key Characteristics | Recommended Treatment |
|---|---|---|
| Chronic Bursitis | Gradual onset, painless swelling | Rest, anti-inflammatory medication, icing |
| Infected Bursitis | Warmth, tenderness, fever | Antibiotics, potential drainage |
| Traumatic Bursitis | Common in athletes, repetitive strain | Rest, compression, targeted therapy |
Treatment depends on the severity and type of bursitis. Most cases improve with rest, ice, compression, and anti-inflammatory drugs6.
In rare cases, surgery might be needed for chronic bursitis that doesn’t respond to usual treatments6.
“Early recognition and appropriate treatment are key to managing bursitis effectively and preventing long-term joint complications.”
Conclusion
Preventing bursitis is vital for an active lifestyle and joint health. Smart strategies can significantly reduce your risk. Use protective gear, practice proper lifting, and take breaks during repetitive activities7.
Exercise and physical activity are crucial for prevention. Start new workouts slowly and warm up before strenuous activities. Listen to your body’s signals to avoid overexertion.
Bursitis risk increases with age and certain medical conditions. Strengthen muscles, maintain a healthy weight, and cushion at-risk joints to protect your bursae7.
Medical research explores new bursitis treatments. Studies have looked into ultrasound-guided shoulder injections and platelet-rich plasma therapies8. For persistent joint pain, consult a healthcare professional.
A doctor can provide a comprehensive evaluation and personalized management plan. Early intervention is key to preventing serious joint damage.
Understand your body’s limits and adopt preventive measures. This approach helps maintain an active, pain-free lifestyle and optimal joint health.
FAQ
What exactly is bursitis?
Where does bursitis most commonly occur?
What are the primary causes of bursitis?
What are the typical symptoms of bursitis?
When should I seek medical attention for bursitis?
How is bursitis typically treated?
Can bursitis be prevented?
How long does bursitis typically last?
Are certain people more at risk for developing bursitis?
Can bursitis cause permanent joint damage?
Source Links
- Bursitis – Symptoms and causes – https://www.mayoclinic.org/diseases-conditions/bursitis/symptoms-causes/syc-20353242
- Arthritis, Bursitis, or Tendonitis: What’s Causing my Pain? – https://www.medstarhealth.org/blog/arthritis-bursitis-tendonitis-whats-causing-pain
- No title found – https://www.arthritis.org/diseases/bursitis
- Patient education: Bursitis (Beyond the Basics) – https://www.uptodate.com/contents/bursitis-beyond-the-basics/print
- Bursitis Causes, Symptoms and Treatment – https://www.piedmont.org/spine/conditions-diseases/spine-bursitis
- Shoulder Bursitis – https://www.hopkinsmedicine.org/health/conditions-and-diseases/shoulder-bursitis
- Diagnosing Bursitis & Tendinitis – https://nyulangone.org/conditions/bursitis-tendinitis/diagnosis
- Bursitis: Practice Essentials, Anatomy, Pathophysiology – https://emedicine.medscape.com/article/2145588-overview