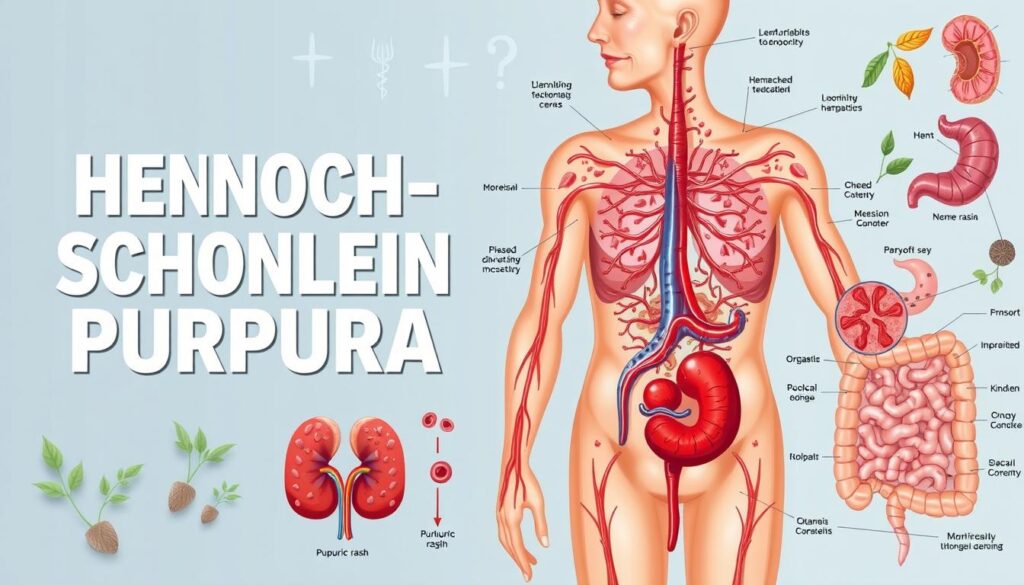
Henoch-Schonlein Purpura (HSP) is a complex autoimmune disorder that affects mainly children. It causes inflammation in small blood vessels, creating unique challenges for patients and doctors1.
HSP mostly occurs in children under 10 years old. It’s slightly more common in boys. The condition can develop after common infections like colds1.
White and Asian children are more likely to get HSP than other groups1. Knowing about HSP can help you spot early signs and get medical help quickly.
Key Takeaways
- HSP is a rare autoimmune disorder affecting primarily children
- The condition involves inflammation of small blood vessels
- Triggers can include respiratory infections and various environmental factors
- Most cases resolve within a month without lasting complications
- Medical monitoring is essential to prevent potential kidney issues
Understanding Henoch-Schonlein Purpura and Its Impact
Henoch-Schonlein Purpura (HSP) is a complex inflammatory disorder. It mainly affects children, presenting unique challenges in diagnosis and management. Families and healthcare providers often struggle with this condition.
What Causes HSP to Develop
HSP develops due to complex immune system responses. Various factors can trigger leukocytoclastic vasculitis, including viral infections and immune system abnormalities2.
HSP is the most common childhood vasculitis. It affects about 20 in 100,000 children2.
Common Risk Factors and Triggers
- Upper respiratory tract infections
- Genetic predisposition
- Cold weather exposure
- Certain medications
- Insect bites
Children ages 2-6 are most often affected by HSP. However, it can occur at any age2.
About one-third of children with HSP experience recurring symptoms2.
How HSP Affects Your Body
HSP can impact multiple body systems. It causes distinct symptoms such as:
- Characteristic purpuric rash on legs and buttocks
- Joint pain and swelling
- Abdominal pain
- Potential kidney involvement
IgA nephropathy is a serious potential complication. Some patients may experience progressive kidney damage3.
HSP can affect joints, kidneys, the gastrointestinal tract, and skin3.
Most children with HSP will ultimately recover completely without long-term consequences2.
Knowing these complexities helps in facing potential challenges. It also aids in seeking appropriate medical support.
Diagnosis and Treatment Options for HSP Management
Henoch-Schonlein Purpura (HSP) requires a thorough understanding of diagnosis and treatment. This autoimmune disorder needs a comprehensive approach for proper care4.
Diagnosis starts with a detailed clinical exam. Doctors look for specific signs, including:
HSP diagnostic tools include comprehensive medical assessments. These may involve urinalysis, blood tests, and possible skin or kidney biopsies.
Treatment aims to manage symptoms and prevent complications. Your doctor might suggest NSAIDs, corticosteroids, or immunosuppressants for severe cases6.
Early intervention is key to managing HSP effectively and preventing long-term kidney complications.
Most children recover from HSP within four weeks6. However, regular check-ups are crucial to monitor potential kidney issues4.
Remember, each HSP case is unique, and personalized medical guidance is crucial for optimal management.
Conclusion
Henoch-Schönlein purpura (HSP) is a complex autoimmune disorder that needs ongoing medical care. This vasculitis affects kids aged 2-11 most, with 70% experiencing joint issues in ankles and knees7.
Renal involvement is crucial in HSP management. Less than 1% of cases progress to end-stage renal disease, but long-term follow-up is vital7. Research shows that many children face kidney-related complications, making proactive medical supervision essential7.
Treatment options are improving, with corticosteroids and azathioprine helping manage severe cases7. Patients should work with doctors to create personalized treatment plans. Half of HSP patients may experience recurrence, highlighting the need for ongoing medical support7.
Dealing with HSP requires patience and teamwork with healthcare providers. Stay informed and attend regular check-ups to manage the disorder effectively. This approach will help you achieve the best long-term health outcomes.
FAQ
What is Henoch-Schonlein Purpura (HSP)?
What are the main symptoms of HSP?
What typically triggers Henoch-Schonlein Purpura?
How is HSP diagnosed?
What treatment options are available for HSP?
Is Henoch-Schonlein Purpura a serious condition?
Can adults develop Henoch-Schonlein Purpura?
How long does HSP typically last?
Source Links
- Henoch-Schonlein purpura-Henoch-Schonlein purpura – Symptoms & causes – Mayo Clinic – https://www.mayoclinic.org/diseases-conditions/henoch-schonlein-purpura/symptoms-causes/syc-20354040
- Henoch-Schonlein Purpura – https://www.chop.edu/conditions-diseases/henoch-schonlein-purpura
- IgA Vasculitis (Henoch-Schönlein Purpura) – StatPearls – https://www.ncbi.nlm.nih.gov/books/NBK537252/
- Henoch-Schönlein purpura in children: Limited benefit of corticosteroids – https://pmc.ncbi.nlm.nih.gov/articles/PMC4229160/
- Clinical Practice Guidelines : Henoch-Schönlein purpura – https://www.rch.org.au/clinicalguide/guideline_index/HenochSchonlein_purpura/
- Henoch-Schonlein Purpura: Causes, Symptoms, and Treatment – https://www.webmd.com/skin-problems-and-treatments/henoch-schonlein-purpura-causes-symptoms-treatment
- Henoch-Schönlein Purpura: A Review – https://www.aafp.org/pubs/afp/issues/1998/0801/p405.html/1000