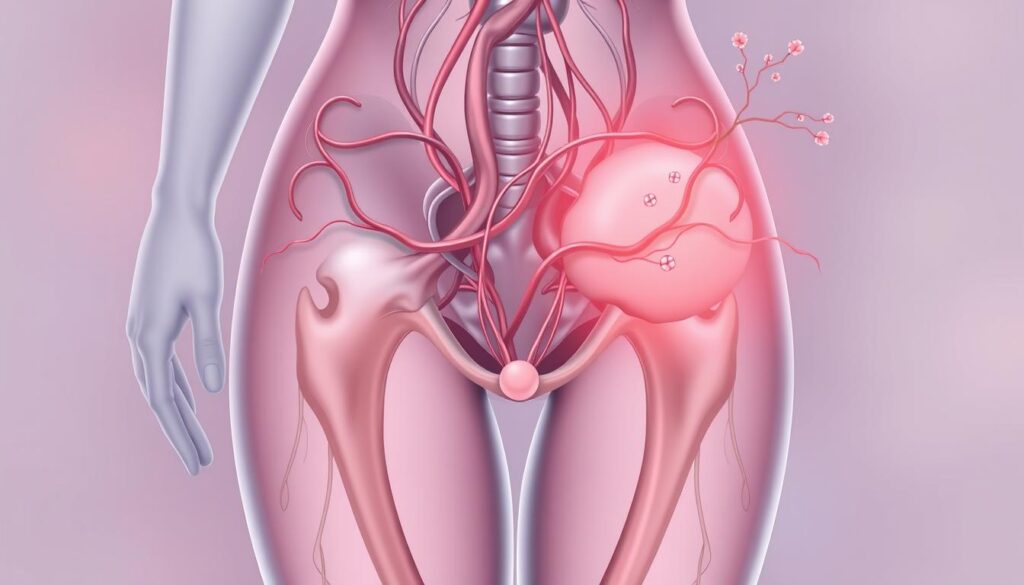
Pelvic congestion syndrome (PCS) can disrupt your sexual health and well-being. It causes complex symptoms that affect intimate relationships1. Many women with unexplained pelvic pain may have this challenging syndrome1.
PCS often leads to painful intercourse, affecting 71% to 78% of patients1. This creates major hurdles in sexual experiences. Postcoital aching and acute pain can make intimacy uncomfortable and distressing1.
PCS is a complex condition with various symptoms. Up to 54% of patients experience menstrual disorders, including heavy and irregular bleeding1. Other common issues are bloating, nausea, and frequent urination1.
Getting professional medical help is vital for managing PCS. About 10 million women have chronic pelvic pain1. Sadly, 7 million avoid seeking help. Understanding your symptoms is key to effective treatment1.
Key Takeaways
- PCS can significantly impact sexual health and intimate relationships
- Painful intercourse affects up to 78% of patients
- Menstrual disorders are common with PCS
- Professional medical consultation is essential for proper diagnosis
- Many women experience chronic pelvic pain without seeking treatment
Preparing for the Disclosure Conversation
Talking about sexual health takes bravery and careful planning. Knowing your STI status is key to responsible sexual behavior. Your approach can greatly affect your well-being and your partner’s understanding2.
Gathering Information About Your STI
Research is vital before discussing your STI status. Learn about your specific infection’s transmission, symptoms, and treatments. Understand its long-term health effects2.
Use reliable medical sources for accurate, current information. This knowledge will help you explain your situation confidently3.
- Transmission methods
- Potential symptoms
- Available treatments
- Long-term health implications2
Choosing the Right Time and Place
Pick a suitable setting for your sexual health talk2. Choose a private, comfy spot when both of you are sober. Avoid sexual situations and allow enough time to talk.
- Choose a private, comfortable location
- Ensure both parties are sober
- Avoid sexual situations during the discussion
- Allow sufficient time for dialogue
The goal is creating a safe, non-threatening environment for open communication.
Managing Your Emotions and Expectations
Getting emotionally ready is crucial for responsible sexual behavior. Your partner might react with shock, anger, or confusion. Stay calm, listen, and provide clear information.
| Potential Reaction | Recommended Response |
|---|---|
| Shock | Remain calm, provide information |
| Anger | Stay compassionate, listen actively4 |
| Confusion | Offer clear, factual explanations |
Practice the conversation beforehand to boost your confidence. This will help you communicate better during STI testing discussions2.
Approaches for Different Relationship Scenarios
STI disclosure can be challenging. Understanding the right approach for different relationships is crucial. It promotes open communication and sexual health.
Your communication strategy should fit the relationship context. Only half of people think they should disclose an STI before sex5. This shows the need for confident disclosure techniques.
Disclosing to a New or Potential Partner
For new partners, direct and timely communication is key. Consider these strategies for STI disclosure:
- Choose a private, comfortable setting
- Be direct and honest about your sexual health status
- Provide accurate information about your specific STI
- Offer resources for additional understanding
Talking to a Current Partner
With a current partner, transparency builds trust. Open dialogue about sexual health can strengthen your relationship. Get tested together and share your results openly6.
| Relationship Stage | Recommended Disclosure Approach |
|---|---|
| New Partner | Direct, before sexual activity |
| Current Partner | Collaborative testing, mutual support |
| Past Partners | Health-focused notification |
Informing Past Sexual Partners
When notifying past partners, focus on health concerns. Inform partners from the last six months if you test positive5. Consider using anonymous notification services if direct contact feels uncomfortable.
Remember, disclosing your STI status is an act of responsibility and care for your sexual health and your partners’.
Over half of Americans will test positive for at least one STI. Approach these talks with empathy and respect. You can help reduce stigma and promote safe sex practices6.
Communication Strategies and Sample Scripts
Talking about sexual health takes bravery and care. Sharing your STD status can impact your partner’s response. Honest talks are key for safe sex practices.
Starting the Conversation
Find a quiet, private place to talk about STIs. Make sure you have enough time. Direct and clear communication is vital7.
- Select a quiet, private location
- Ensure enough time for discussion
- Approach the conversation with empathy
Handling Questions and Concerns
Be ready to answer your partner’s questions about your STI status. Offer facts and helpful resources. Cover these important points:
- Transmission risks
- Treatment options
- Prevention strategies
Remember, transparency builds trust in sexual health conversations.
Discussing Next Steps and Prevention
Managing sexual health requires prevention. Some STIs need antibiotics, while others can’t be fully cured7. Work together to create a prevention plan8.
| Prevention Strategy | Effectiveness |
|---|---|
| Condom Use | Limited Protection |
| Regular Testing | High Importance |
| Open Communication | Critical for Safety |
Being honest about your STD status shows respect. It protects your partner’s health and strengthens your bond8.
Promoting Regular STI Testing and Prevention
Taking charge of your sexual health requires proactive strategies. STI testing plays a crucial role in maintaining wellness. It protects you and your partners9.
From 2014 to 2019, STIs in the U.S. increased significantly. Chlamydia rose 19%, gonorrhea 56%, and syphilis 74%. These numbers highlight the importance of regular screening9.
Safe sex practices are vital for reducing transmission risk. Implementing comprehensive STI prevention strategies can protect your sexual health10. Condoms are highly effective against STIs when used correctly10.
Vaccines are available for certain STIs like hepatitis B and HPV. They offer additional protection for sexually active individuals10.
Establishing a Routine for STI Screenings
Schedule annual screenings and get tested before engaging with new partners. Chlamydia screening rates have improved in some healthcare providers. Coverage increased from 55% to 72%11.
Expedited partner therapy has become an effective strategy. Usage rates in urban clinics rose from 20% to 48%11.
Practicing Safe Sex and Risk Reduction
Behavioral counseling and comprehensive sexuality education are crucial for STI prevention10. Discuss sexual health openly with your partners. Consider getting tested together to ensure mutual health and safety9.
Most STIs are treatable. Early detection can prevent potential long-term health complications.
Building a Culture of Openness in Relationships
Trust and communication are key to sexual health. Approach STI testing discussions with empathy and understanding. Avoid judgment to create a supportive environment.
Normalizing these conversations helps reduce stigma. It also promotes responsible sexual behavior.
FAQ
How do I know when it’s the right time to disclose my STI status?
What if I’m nervous about telling my partner about my STI?
How should I actually start the conversation about my STI?
What if my partner reacts negatively to my disclosure?
Do I legally have to disclose my STI status?
How can I prevent transmitting my STI to my partner?
What if I want to tell a past partner about an STI?
Source Links
- Current Concepts of Pelvic Congestion and Chronic Pelvic Pain – https://pmc.ncbi.nlm.nih.gov/articles/PMC3015423/
- STD Results Aren’t “Clean” or “dirty” They are Positive or Negative – https://www.stdcheck.com/blog/expert-tips-on-respectfully-disclosing-your-std-status/
- Guide to Taking a Sexual History – https://www.cdc.gov/sti/hcp/clinical-guidance/taking-a-sexual-history.html
- Disclosure and HIV – https://www.thewellproject.org/hiv-information/disclosure-and-hiv
- Tips for disclosing you have an STI, including anonymous ways to share – https://www.abc.net.au/news/2024-10-11/tips-for-disclosing-you-have-an-sti/104416154
- Disclosing Your STI Status: How and Why to Do It | Psych Central – https://psychcentral.com/health/disclosing-sti-status
- How To Talk About STIs With Your Clients – https://www.instituteforrelationalintimacy.com/blog/how-to-talk-about-stis-with-your-clients
- Section 1: Developing Documents for a Patient Notification – https://www.cdc.gov/healthcare-associated-infections/hcp/patient-notification-toolkit/developing.html
- Sexually Transmitted Infections: Updates From the 2021 CDC Guidelines – https://www.aafp.org/pubs/afp/issues/2022/0500/p514.html
- Prevention – https://www.who.int/teams/global-hiv-hepatitis-and-stis-programmes/stis/prevention
- STD Prevention Policies in the United States: Evidence and Opportunities – https://pmc.ncbi.nlm.nih.gov/articles/PMC5283689/