Pectus excavatum is a chest wall deformity affecting 1 in 200 people. This cardiothoracic abnormality has a strong genetic link1. The sunken chest appearance can impact your daily life and overall well-being1.
Males are more likely to have pectus excavatum. It occurs five times more often in boys than in girls1. Many people with this condition manage their symptoms well.
Living with pectus excavatum can be challenging. You might feel short of breath, have chest pain, or get tired easily1. These physical issues can affect your self-esteem and social life1.
Key Takeaways
- Pectus excavatum is a common chest wall deformity affecting 1 in 200 people
- The condition is more prevalent in males
- Genetic factors play a significant role in its occurrence
- Symptoms can be both physical and psychological
- Multiple treatment options are available
Understanding Pectus Excavatum: Causes and Symptoms
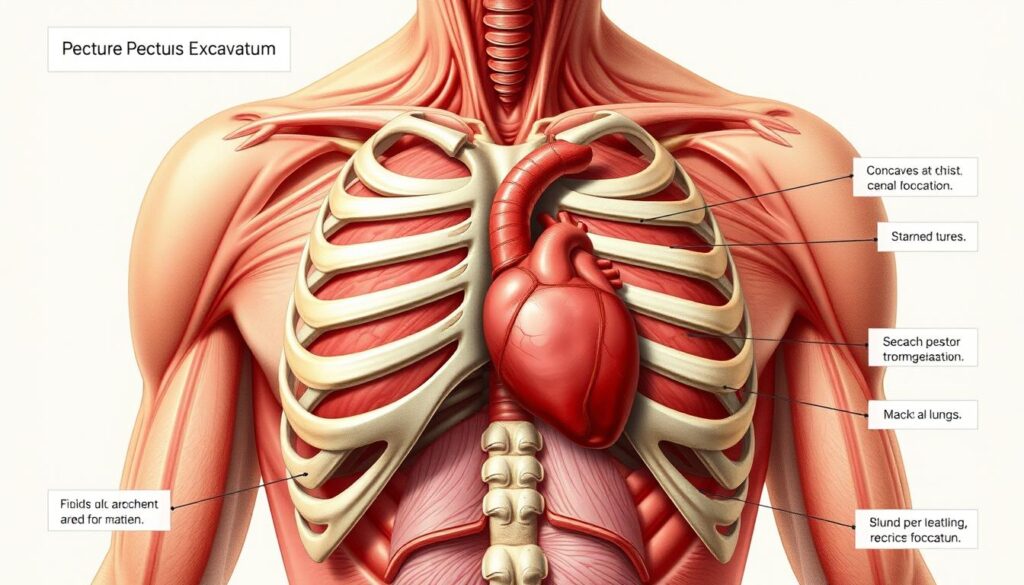
Pectus excavatum is a chest wall deformity that affects physical and emotional well-being. It creates a noticeable depression in the chest, making it appear sunken or concave2.
Defining the Condition
This deformity occurs when the breastbone grows abnormally inward. It creates a hollow in the chest. Pectus excavatum affects males more often, with a 3:1 male-to-female ratio2.
Genetic Links and Risk Factors
The exact cause is unclear, but there’s a strong genetic component. Key risk factors include potential genetic inheritance and association with Marfan syndrome.
Pectus excavatum may also link to other connective tissue disorders. Children with this condition might face additional health challenges.
| Associated Condition | Prevalence |
|---|---|
| Scoliosis | Approximately 15% |
| Mitral Valve Prolapse | 15-20% |
Recognizing Symptoms
Symptoms can range from mild to severe. You might experience shortness of breath, chest pain, or a rapid heartbeat.
Decreased exercise tolerance and fatigue are also common. The condition typically worsens during adolescent growth spurts3.
- Shortness of breath
- Chest pain
- Rapid heartbeat
- Decreased exercise tolerance
- Fatigue
In extreme cases, pectus excavatum can potentially compress heart and lung function3.
Understanding your body and seeking professional medical advice is crucial for managing pectus excavatum effectively.
Treatment Options and Medical Interventions
Pectus excavatum offers various treatment options to enhance appearance and breathing. Your specific plan will be based on your condition’s severity and health factors4.
For mild cases, non-surgical methods can be effective. These include vacuum bell therapy, physical therapy, and bracing treatment.
- Vacuum bell therapy5
- Physical therapy to strengthen chest muscles
- Bracing treatment to support chest wall development
The vacuum bell device can reshape the chest wall, especially in younger patients5. Noticeable changes may take 3-6 months to appear.
Severe cases may require surgery. Two main surgical procedures are available:
| Procedure | Technique | Recovery |
|---|---|---|
| Nuss Procedure | Minimally invasive, two small chest incisions, curved steel bar placement | 2-3 years for permanent chest reshaping5 |
| Ravitch Procedure | Single large chest incision, cartilage removal, metal support placement | Longer recovery, comprehensive chest wall reconstruction |
New techniques like cryoablation have improved post-surgical pain management4. This method freezes chest wall nerves to reduce discomfort.
Consulting a chest wall surgeon is crucial to determine the most appropriate treatment strategy for your specific condition5.
Conclusion
Pectus excavatum can affect your life quality, but modern medicine offers solutions. Chest wall surgery has advanced, providing effective treatments for this condition6. The best age for surgery is between 12 and 18 years, with minimally invasive techniques showing great results6.
Surgical options have high success rates, improving heart and lung function7. About 66% of patients with exercise limits see major improvements after surgery7. Most patients return to normal activities within two to three weeks6.
Your treatment plan depends on your unique situation. Modern techniques like the Nuss procedure and modified Ravitch repair work well for both kids and adults6. A specialized chest wall surgeon can help you choose the best approach8.
Pectus excavatum affects about 1 in 1,000 children, mostly males7. With proper medical care, you can improve your health and boost your confidence.
FAQ
What is pectus excavatum?
What causes pectus excavatum?
What are the common symptoms of pectus excavatum?
How is pectus excavatum diagnosed?
What are the treatment options for pectus excavatum?
Is surgery always necessary?
What is the Nuss procedure?
Can pectus excavatum affect my quality of life?
Source Links
- Living With Mild Pectus Excavatum – https://healthcare.utah.edu/healthfeed/2024/03/living-mild-pectus-excavatum
- Pectus Excavatum | Symptoms, Diagnosis & Treatment – https://www.cincinnatichildrens.org/health/p/pectus-excavatum
- Pectus excavatum – Symptoms and causes – https://www.mayoclinic.org/diseases-conditions/pectus-excavatum/symptoms-causes/syc-20355483
- Laryngeal Cancer Treatments – https://stanfordhealthcare.org/medical-conditions/blood-heart-circulation/pectus-excavatum/treatments.html
- Chest Wall Disorder: Pectus Excavatum (for Parents) – https://kidshealth.org/en/parents/pectus-excavatum.html
- Pectus Excavatum | Columbia Surgery – https://columbiasurgery.org/conditions-and-treatments/pectus-excavatum
- Pectus Excavatum – https://www.wakemed.org/wakemed-physician-practices/specialties/pediatric-surgery/services-and-specialties/pectus-excavatum
- Pectus excavatum and carinatum: a narrative review of epidemiology, etiopathogenesis, clinical features, and classification – https://jtd.amegroups.org/article/view/82552/html