Pelvic organ prolapse is a widespread women’s health issue. National estimates show a 2.9% prevalence, with some surveys indicating up to 8%1. Around 300,000 surgeries tackle this problem annually in the US1.
For those facing pelvic organ prolapse, knowing your options is vital. Mesh implants offer a potential fix for weakened pelvic floor muscles. Women have a 11-19% lifetime risk of needing surgery for pelvic floor disorders1.
Mesh implants have a rocky history. From 2004 to 2008, reports of issues with synthetic vaginal mesh soared five-fold1. Thousands of patients have sued over potential side effects2.
Medical experts acknowledge the complex nature of mesh implants. The American College of Obstetricians and Gynecologists and other groups continue to guide this sensitive treatment1.
Key Takeaways
- Pelvic organ prolapse affects 2.9-8% of women nationally
- Annual prolapse surgeries in the US exceed 300,000
- Mesh implants carry potential risks and complications
- Medical guidelines continue to evolve around mesh technology
- Patient awareness is crucial when considering prolapse repair
What Are Mesh Implants?
Surgical mesh has transformed pelvic floor disorder treatment. It offers a new solution for prolapse and related conditions. Understanding mesh composition and uses is vital when considering this option.
Mesh implants are special medical devices that provide support in surgeries. These screen-like materials reinforce weak tissues. They help restore normal body functions3.
Overview of Mesh Technology
Modern mesh technology has key features:
- Synthetic polymers that can be non-absorbable or absorbable
- Biologic materials derived from animal tissues
- Composite materials combining multiple technologies
Mesh implant surgery recovery varies based on the type used4. Each patient’s healing experience is unique.
Types of Mesh Used in Surgery
Doctors use four main mesh categories:
- Non-absorbable synthetic mesh: Primarily made of polypropylene
- Absorbable synthetic mesh: Constructed from polyglycolic acid
- Biologic mesh: Derived from animal collagen sources
- Composite mesh: Combining multiple material technologies
Understanding mesh types helps patients make informed decisions about their surgical options.
Surgical mesh for prolapse repair is always improving. Ongoing research enhances patient outcomes. It also reduces potential complications3.
Understanding Prolapse Disorders
Pelvic organ prolapse affects many women’s quality of life. It happens when pelvic floor muscles and tissues weaken. This causes organs to shift from their normal positions5.
Recognizing potential symptoms is crucial. It helps you seek proper treatment for pelvic organ prolapse.
Types of Pelvic Organ Prolapse
Several types of pelvic organ prolapse can occur, depending on which organs are affected:
- Bladder prolapse (cystocele)
- Uterine prolapse
- Rectal prolapse (rectocele)
- Vaginal vault prolapse
- Urethral prolapse
Common Symptoms
Identifying symptoms of pelvic organ prolapse is key for early intervention. Women may experience:
- Feeling of pelvic pressure or fullness
- Urinary incontinence
- Difficulty with bowel movements
- Painful sexual intercourse
- Visible bulging from the vaginal area
Mesh implants can be an effective treatment for severe or recurring prolapse cases5. However, 8-15% of women might face complications after surgery5.
It’s crucial to weigh the risks and benefits. This helps you make an informed decision about your health6.
“Knowledge is the first step towards effective treatment and management of pelvic organ prolapse.”
Risk factors for developing pelvic organ prolapse include:
- Multiple pregnancies
- Vaginal childbirth
- Aging
- Chronic coughing
- Obesity
Your doctor can help identify your specific condition type and severity. They’ll guide you towards the most suitable treatment options7.
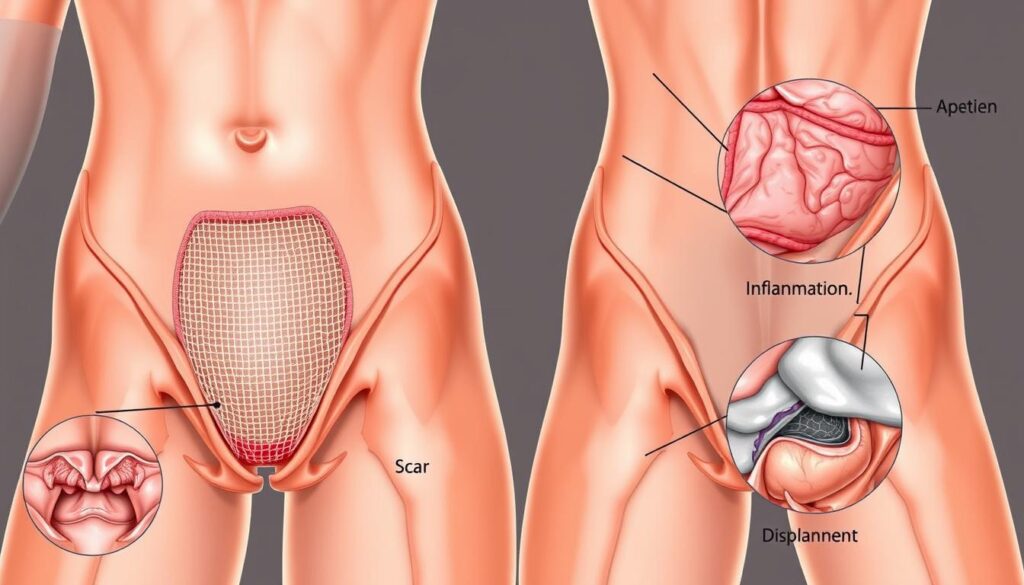
The Role of Mesh in Prolapse Repair
Mesh implants have revolutionized pelvic organ prolapse surgery. These devices offer a sophisticated approach to weakened pelvic tissues. They provide crucial structural support for patients8.
Mechanism of Action
Mesh implants reinforce weak pelvic floor muscles and provide extra support. They prevent tissue sagging and restore normal anatomical positioning. The mesh acts as a supportive scaffold8.
This innovative approach helps reduce the risk of recurring prolapse. It’s designed to maintain proper pelvic organ positioning long-term.
- Reinforces vaginal wall structures
- Provides additional tissue support
- Helps maintain proper pelvic organ positioning
Benefits of Using Mesh
Mesh implants offer several advantages for patients with pelvic organ prolapse. About 300,000 surgical procedures using this technique are performed annually. This shows its widespread acceptance and effectiveness8.
| Benefit | Description |
|---|---|
| Reduced Recurrence | Lower prolapse recurrence rates compared to traditional surgical methods |
| Improved Support | Enhanced structural reinforcement for pelvic tissues |
| Surgical Precision | More targeted approach to addressing prolapse issues |
Mesh technology represents a significant advancement in surgical options for pelvic organ prolapse, offering patients new hope for effective treatment.
Mesh implants show promising results, but they come with potential risks. Patients should discuss these thoroughly with their healthcare provider. The FDA cleared surgical mesh for pelvic organ prolapse in 20018.
Learning about mesh implants can help you make informed decisions. Understanding their mechanism and benefits is crucial. This knowledge will guide your choice in prolapse repair options9.
The Surgical Procedure for Mesh Implants
Mesh implants are crucial for treating pelvic organ prolapse and stress urinary incontinence. Knowing the procedure details helps you choose the best surgical option for your condition10.
Surgical Approach and Preparation
Doctors use specific techniques for mesh implant surgery based on your condition. These procedures usually happen in hospitals under anesthesia10. Your medical team will pick the best approach for you.
Types of Surgical Mesh Procedures
- Transvaginal mesh for pelvic organ prolapse
- Transabdominal mesh repair
- Mesh sling procedure for stress urinary incontinence
Surgical mesh comes in various materials, including synthetic options for permanent support. It can be knitted or non-knitted, absorbable, non-absorbable, or a mix11.
Recovery Timeline
Mesh implant surgery recovery typically takes about three weeks10. During this time, patients should:
- Follow strict post-operative instructions
- Attend follow-up appointments
- Gradually resume normal activities
- Monitor for any potential complications
Surgical mesh can help with prolapse symptoms, but it’s important to know the possible risks10.
Important Considerations
The FDA has taken action regarding surgical mesh. In 2016, they classified transvaginal mesh for prolapse as high-risk11. Currently, no FDA-approved transvaginal mesh products for prolapse repair are sold in the U.S11.
| Procedure Type | Typical Recovery Time | Potential Risks |
|---|---|---|
| Transvaginal Mesh | 3-4 weeks | Mesh erosion, infection |
| Mesh Sling | 2-3 weeks | Urinary problems, pain |
Recovering from mesh implant surgery takes time and good communication with your doctor. Always talk about all potential risks and benefits before deciding on surgery.
Potential Risks and Complications
Vaginal mesh implants for pelvic organ prolapse repair come with potential risks. Patients should carefully evaluate these complications with their healthcare providers. Understanding these risks is vital for making an informed decision.
In 2010, about 300,000 women had pelvic organ prolapse repair. Surgical mesh was used in one-third of these procedures12. The surgery can be beneficial but has significant potential side effects.
Common Side Effects
- Vaginal mesh erosion
- Chronic pelvic pain
- Infection
- Bleeding
- Painful sexual intercourse
Serious Complications to Consider
Mesh erosion through the vaginal wall is a common side effect. Over 50% of women with erosion needed surgical removal12. Erosion rates vary significantly:
| Procedure Type | Mesh Erosion Rate |
|---|---|
| SUI Slings | Approximately 2% |
| Sacrocolpopexy | 1.9% – 5% |
Critical Warning: In April 2019, the FDA banned transvaginal mesh for pelvic organ prolapse treatment1213. This ban was due to increased negative effects.
Patients should thoroughly discuss potential pelvic organ prolapse mesh complications with their surgeon before proceeding with any surgical intervention.
Other serious complications can include:
- Organ perforation
- Fistula formation
- Neuromuscular problems
- Recurrent prolapse
Knowing these risks helps you make an informed decision. You’ll be better equipped to choose the right treatment options for your health.
Patient Experiences with Mesh Implants
Mesh implant surgeries can be complex and challenging for patients. Understanding real experiences is crucial when dealing with pelvic organ prolapse mesh complications. Your journey requires careful thought and consideration.
Recovery from mesh implant surgery varies widely among patients. Real stories show both successes and significant challenges. Reports of vaginal mesh complications rose sharply between 2005 and 201014.
Patient Case Studies
Mesh implant surgeries involve various aspects of patient experiences. These include initial symptoms, potential interventions, and removal procedures.
- 78% of patients initially presented with stress urinary incontinence14
- Approximately 1 in 30 women may require additional surgical interventions within 10 years14
- Mesh removal procedures show complex outcomes, with some patients needing complete or partial mesh removal14
Success Rates and Complications
“Patient experiences demonstrate that individual outcomes can significantly differ from general medical statistics.”
Urinary incontinence mesh surgeries often have high success rates. However, prolapse surgeries come with higher risks of complications2. Thousands of lawsuits highlight potential issues with mesh implants2.
| Procedure Type | Complication Risk | Patient Satisfaction |
|---|---|---|
| Urinary Incontinence Mesh | Low | High |
| Vaginal Prolapse Mesh | High | Variable |
Your mesh implant surgery recovery depends on several factors. Consulting experienced urogynecological specialists is crucial. They can help you understand potential risks and benefits2.
Alternatives to Mesh Implants
Prolapse repair offers several options beyond traditional mesh implants. Learning about these alternatives can help you choose the best pelvic health treatment.
Modern medicine provides effective approaches for prolapse repair without mesh. These methods can address your specific medical needs15. The aim is to find a solution that reduces risks and offers long-term relief.
Traditional Surgical Methods
Surgeons now recommend various traditional surgical approaches for prolapse repair without mesh:
- Native tissue repair using patient’s own tissues16
- Burch colposuspension procedure15
- Fascial sling surgeries15
“Non-mesh surgical alternatives provide effective treatment with reduced complications” – Dr. Ajay Singla15
Non-Surgical Options
Several non-invasive options exist for those seeking alternatives to mesh implants:
- Pelvic floor muscle exercises15
- Physical therapy targeting pelvic muscles
- Pessary devices for structural support
- Lifestyle modifications
Conservative approaches are often the first step before considering surgery15. Your doctor can help you find the best alternatives to mesh implants for your condition.
Always consult with a specialized urogynecologist to explore the most appropriate prolapse repair options for your specific situation.
Informed Consent and Patient Education
Mesh implant surgery for prolapse repair requires thorough understanding of informed consent. Your healthcare journey needs complete knowledge about potential risks and treatment options. It’s crucial to be well-informed before making any decisions.
Recovering from mesh implant surgery needs careful planning and open talks with your doctor. The risks of these implants are significant. It’s important to evaluate them carefully.
Importance of Discussing Risks
Patients must have clear talks about possible complications. Key risks to explore include:
- Potential surgical complications
- Long-term mesh-related challenges
- Impact on future surgical interventions17
“Your right to comprehensive information is crucial in making an informed medical decision.” – Medical Ethics Guidelines
Questions to Ask Your Surgeon
Prepare a list of key questions about the mesh implant procedure:
- What specific type of mesh will be used?
- What are the potential long-term complications?
- Are there alternative treatment options?
- How might this procedure affect future surgeries18?
Doctors now recognize the need for detailed patient consent. The Montgomery v Lanarkshire Health Board case set new standards. It requires doctors to discuss material risks and alternatives openly17.
Grasping the complexities of mesh implant surgery is vital. It helps you make informed choices about your health. Your recovery process depends on this knowledge19.
Current Regulations and Guidelines
Medical rules for pelvic organ prolapse surgery are complex. They ensure patient safety with mesh implants. The medical community is working to address challenges with these technologies.
The FDA has changed mesh implant rules to protect patients. In 2011, major shifts happened in mesh use20:
- Before 2011, 90% of urogynecologists used transvaginal mesh implants
- After 2011, only 61% continued using these implants
FDA Recommendations and Quality Control
Strict rules now guide mesh implant makers and doctors. Key areas include:
- Specialized surgeon training
- Careful patient selection
- Vigilant post-operative monitoring
Global agencies took action in December 201721:
- Australia banned transvaginal mesh products
- The UK recommended using mesh only in research contexts
- New Zealand requested manufacturers to provide safety evidence
Reporting and Incident Management
The Medical Device Coordination Group set up reporting rules for mesh makers22. These rules require:
- Reporting serious incidents to competent authorities
- Periodic summary reporting of device-related events
- Tracking statistically significant complications
Patient safety remains the paramount concern in mesh implant lawsuit updates and regulatory considerations.
By 2050, over 50 million women may have pelvic floor problems20. Ongoing research and new rules will help address these medical needs.
Ongoing Research and Developments
Pelvic organ prolapse treatment is evolving rapidly. Researchers are exploring innovative surgical options for better patient outcomes. Medical professionals are developing the best treatment through advanced medical investigations.
Breakthrough Studies on Mesh Efficacy
Recent research has revealed key insights into mesh technologies. A comprehensive review of 2,816 articles highlighted the complexity of current research23.
Initial success rates for mesh procedures range from 87% to 95%. However, complications remain a significant concern23.
- Global incidence of pelvic organ prolapse reaches 13 million new cases annually23
- Surgical interventions are chosen by approximately 19% of diagnosed women23
- Recurrence rates after surgical management range from 10% to 30%23
Innovative Approaches in Prolapse Repair
Research on prolapse repair has grown dramatically. In 2010, there were only 3 publications. By 2021, this number jumped to 26624.
Scientists are now focusing on creating biocompatible materials. They’re also developing advanced tissue engineering techniques to reduce surgical risks.
| Research Metric | Value |
|---|---|
| Total Articles Reviewed | 2,816 |
| Total Citations | 39,850 |
| Mean Citations per Article | 15.6 |
The future of prolapse repair lies in personalized, minimally invasive approaches that prioritize patient safety and long-term outcomes.
New surgical options for pelvic organ prolapse are on the horizon. These will focus on reducing complications and improving treatment effectiveness.
Conclusion: Making Informed Choices
Understanding mesh implants for prolapse repair is vital. It’s crucial to weigh the risks and benefits carefully. Your health journey demands a thorough evaluation of all treatment options.
Mesh implant risks can vary widely. Complications may include mesh erosion and potential organ injuries25. It’s important to discuss these with specialized healthcare providers.
Recent studies show varying success rates for pelvic organ prolapse surgeries. Reoperation risks range from 1.5% to 13%26. A thorough review of mesh implant techniques highlights the need for patient-specific considerations27.
Your health and comfort should be the top priority. Explore all available options, including non-surgical alternatives. Understanding the potential risks will help you make an informed decision.
Regular follow-ups are key to ensuring the best outcome. Keep open communication with your healthcare team. Monitor any post-surgical symptoms proactively.
FAQ
What is a mesh implant for pelvic organ prolapse?
What conditions can surgical mesh treat?
What are the common risks associated with mesh implants?
Are mesh implants still used for pelvic organ prolapse?
What alternatives exist to mesh implant surgery?
How long is the recovery after mesh implant surgery?
What questions should I ask my surgeon before mesh implant surgery?
Can mesh implants be removed if complications occur?
Are mesh implants covered by insurance?
What ongoing research is being conducted about mesh implants?
Source Links
- Indications, Contraindications, and Complications of Mesh in Surgical Treatment of Pelvic Organ Prolapse – https://pmc.ncbi.nlm.nih.gov/articles/PMC3644007/
- Is Pelvic Mesh Safe? What Patients Need to Know – https://www.michiganmedicine.org/health-lab/pelvic-mesh-safe-what-patients-need-know
- Risks and benefits of mesh in pelvic floor reconstruction – https://www.mayoclinic.org/diseases-conditions/pelvic-organ-prolapse/in-depth/transvaginal-mesh-complications/art-20110300
- Mesh implants have similar outcomes to hysterectomy for vaginal prolapse repair – https://www.nih.gov/news-events/news-releases/mesh-implants-have-similar-outcomes-hysterectomy-vaginal-prolapse-repair
- PDF – https://www.health.nsw.gov.au/sabs/Publications/patients-considering-mesh-implant.pdf
- Explaining the vaginal mesh controversy – https://medicine.uq.edu.au/article/2017/06/explaining-vaginal-mesh-controversy
- Mesh–related and intraoperative complications of pelvic organ prolapse repair – https://pmc.ncbi.nlm.nih.gov/articles/PMC4165670/
- The Role of Vaginal Mesh Procedures in Pelvic Organ Prolapse Surgery in View of Complication Risk – https://pmc.ncbi.nlm.nih.gov/articles/PMC3771437/
- FDA’s Activities: Urogynecologic Surgical Mesh – https://www.fda.gov/medical-devices/urogynecologic-surgical-mesh-implants/fdas-activities-urogynecologic-surgical-mesh
- Surgical Mesh | Pioneer Valley Urology – https://www.pvurology.org/surgical-mesh.php
- Urogynecologic Surgical Mesh Implants – https://www.fda.gov/medical-devices/implants-and-prosthetics/urogynecologic-surgical-mesh-implants
- Surgical Mesh: Use and Complications in Women – https://my.clevelandclinic.org/health/articles/16298-surgical-mesh-use-and-complications-in-women
- Pelvic Organ Prolapse (POP): Surgical Mesh Considerations – https://www.fda.gov/medical-devices/urogynecologic-surgical-mesh-implants/pelvic-organ-prolapse-pop-surgical-mesh-considerations-and-recommendations
- When things go wrong: experiences of vaginal mesh complications – https://pmc.ncbi.nlm.nih.gov/articles/PMC10287809/
- Non-Mesh Options for Stress Urinary Incontinence – https://advances.massgeneral.org/urology/article.aspx?id=1388
- Alternative to Transvaginal Mesh | FEMselect – https://www.femselect.com/a-new-era-of-urogynecology-an-alternative-to-transvaginal-mesh/
- Informed consent checklists for midurethral slings: a common-sense approach – https://pmc.ncbi.nlm.nih.gov/articles/PMC5655583/
- Overview of patient safety issues related to surgical mesh – https://www.patientsafetylearning.org/blog/redress-research-and-regulatory-reform-are-still-needed-an-overview-of-patient-safety-issues-related-to-surgical-mesh
- Management of Mesh and Graft Complications in Gynecologic Surgery – https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2017/04/management-of-mesh-and-graft-complications-in-gynecologic-surgery
- The international discussion and the new regulations concerning transvaginal mesh implants in pelvic organ prolapse surgery – https://pmc.ncbi.nlm.nih.gov/articles/PMC7497328/
- Update on Vaginal Mesh for Prolapse and Incontinence – President’s Perspective – News – https://www.augs.org/update-on-vaginal-mesh-for-prolapse-and-incontinence/
- MDCG Guidance on Vigilance System for Urogynecological Surgical Mesh Implants – https://www.regdesk.co/mdcg-guidance-on-vigilance-system-for-urogynaecological-surgical-mesh-implants/
- Complications of Pelvic Prolapse Surgery Using Mesh: A Systematic Review – https://www.mdpi.com/2075-4426/14/6/622
- Frontiers | Knowledge mapping and visualization analysis of pelvic organ prolapse repair with mesh from 2001 to 2021 – https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2023.1104724/full
- Surgical mesh implants – https://www.baus.org.uk/_userfiles/pages/files/Patients/CBP-8108.pdf
- To mesh or not to mesh: a review of pelvic organ reconstructive surgery – https://pmc.ncbi.nlm.nih.gov/articles/PMC4386830/
- Precision in Practice: The Critical Role of Mesh and Procedure Type Specification in Urogynecological Surgeries and Research – https://pmc.ncbi.nlm.nih.gov/articles/PMC11420388/