Spine surgery can be tough, but spinal fusion offers hope for chronic back problems. This guide explains vertebral fusion, helping you grasp this complex spine surgery1.
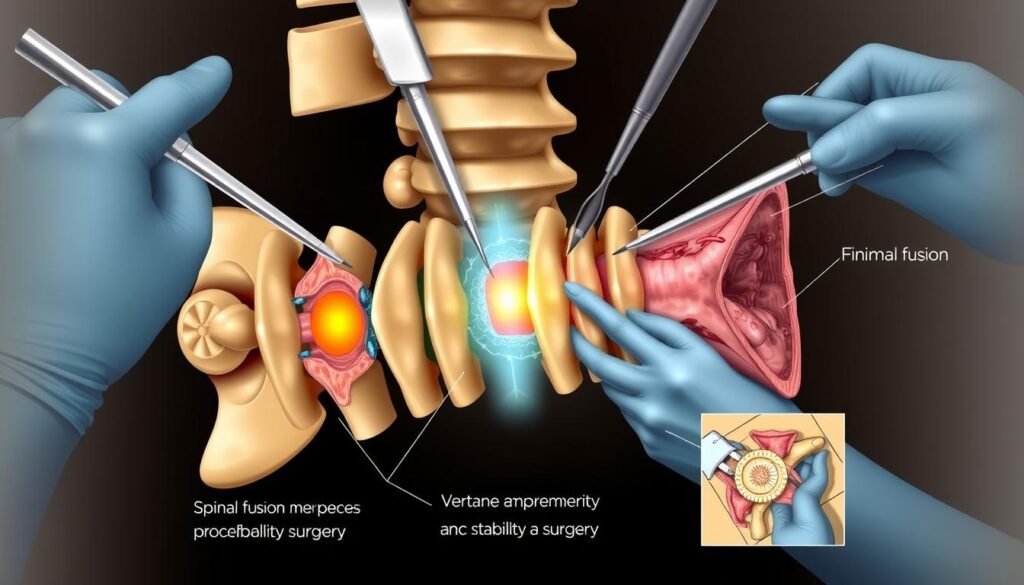
Spinal fusion permanently joins two or more vertebrae in your spine. It eliminates painful motion and boosts stability, addressing various spinal conditions2.
Before surgery, your team will assess if spinal fusion suits your condition. The procedure places bone material between vertebrae, often using metal hardware for alignment2.
Key Takeaways
- Spinal fusion connects vertebrae to reduce pain and increase stability
- The surgery can treat multiple spine-related conditions
- Recovery typically requires several months of healing
- Potential complications exist and should be discussed with your surgeon
- Physical therapy plays a crucial role in post-surgical recovery
What Is Spinal Fusion and How Does It Work
Spinal fusion joins two or more vertebrae into a single structure. It treats various spine issues by stopping movement between affected vertebrae. This surgery stabilizes the spine and addresses chronic pain3.
Doctors may suggest Intervertebral Body Fusion when other treatments fail. This surgery joins vertebrae to prevent nerve stretching. It aims to provide relief from ongoing pain3.
Types of Spinal Fusion Approaches
Surgeons can perform Lumbar Fusion and Cervical Fusion using different methods:
- Anterior approach (from the front)
- Posterior approach (from the back)
- Lateral approach (from the side)
- Minimally invasive techniques
Common Reasons for Spinal Fusion Surgery
Spinal fusion may help with symptoms from various conditions, including:
- Degenerative disk disease
- Spondylolisthesis
- Spinal stenosis
- Scoliosis
- Fractured vertebrae
- Spinal infections
- Herniated disks
- Spinal tumors
Bone Grafting Methods and Materials
Successful Disc Replacement and spinal fusion rely on effective bone grafting. Surgeons use various materials to help bones grow together.
| Graft Type | Description |
|---|---|
| Autografts | Bone material harvested from the patient’s own body |
| Allografts | Bone material from cadaver donors |
| Synthetic Grafts | Artificial bone substitutes |
Doctors may use plates, screws, and rods to stabilize the fusion site. This internal fixation can boost healing potential3.
Your surgical team will determine the most appropriate approach based on your specific spinal condition and overall health.
Preparing for Your Spinal Fusion Surgery
Careful planning is key for Minimally Invasive Spinal Fusion success. Your prep starts weeks before the Spinal Arthrodesis procedure. This ensures the best possible outcome for your surgery.
Your medical preparation is vital. You’ll need a thorough pre-op physical exam. This may include several tests.
Managing your meds is crucial for surgery readiness. Your doctors will guide you on which meds to stop or continue. Certain drugs like Aspirin and Ibuprofen can thin your blood and must be discontinued before surgery5.
“Proper preparation is key to a successful surgical outcome” – Spine Surgery Specialists
Lifestyle changes are a must. If you smoke, quitting is strongly advised. Smoking can greatly reduce fusion success rates. Fusions fail in 40% of smokers, compared to only 8% of non-smokers5.
Staying hydrated before surgery is important. Doctors suggest drinking 8 to 10 glasses of fluid every day5. You’ll get specific instructions on pre-op tasks.
- Fasting before surgery
- Bathing with special antimicrobial soap6
- Removing jewelry and personal items
On surgery day, bring essential documents. Have a support person with you. They can help you through the Minimally Invasive Spinal Fusion process4.
Conclusion
Spine surgery, specifically vertebral fusion, can dramatically improve your life quality. It offers relief for many, but understanding potential outcomes is crucial. Up to 40% of patients may still experience pain a decade after their procedure7.
Your surgery’s success depends on precise techniques and thorough post-operative care. Your recovery journey will be unique. Some patients might need revision surgery, with a 7.5% chance within ten years7.
Certain conditions may require lumbar fusion surgery8. These include trauma-related vertebral displacement and spinal infections. Physical therapy and patient commitment are vital for optimal rehabilitation.
Before choosing spinal fusion, have in-depth talks with your healthcare provider. Review all surgical options and potential outcomes. Understanding the risks and benefits will help you make an informed decision about your spine health.
FAQ
What exactly is spinal fusion surgery?
What conditions can spinal fusion help treat?
How long does recovery from spinal fusion typically take?
Will spinal fusion limit my mobility?
What types of bone grafting materials are used in spinal fusion?
How should I prepare for spinal fusion surgery?
Are there different approaches to spinal fusion?
What are the potential risks of spinal fusion surgery?
Source Links
- Spinal fusion – Mayo Clinic – https://www.mayoclinic.org/tests-procedures/spinal-fusion/about/pac-20384523
- Spinal Fusion: A Valuable Treatment Option – https://my.clevelandclinic.org/health/treatments/25168-spinal-fusion
- Spinal Fusion – OrthoInfo – AAOS – https://orthoinfo.aaos.org/en/treatment/spinal-fusion/
- PDF – https://www.hopkinsmedicine.org/-/media/neurology-neurosurgery/documents/spine/spine-surgery-guide-bayview.pdf
- Preparing for Lumbar Spinal Fusion – https://mayfieldclinic.com/pe-fusionpreparing.htm
- Lumbar Spinal Fusion: Before Your Surgery – https://myhealth.alberta.ca/Health/aftercareinformation/pages/conditions.aspx?hwid=zx4093
- 10 Years After Spinal Fusion: Studies and Research | Premia Spine – https://premiaspine.com/10-years-after-spinal-fusion-studies-and-research/
- ISASS Policy Statement – Lumbar Spinal Fusion – https://isass.org/isass-policy-statement-on-lumbar-spinal-fusion-surgery/