Molar Pregnancy is a rare and complex pregnancy complication. It involves abnormal growth of placental tissue, disrupting typical pregnancy development1. Knowing about this condition can help you understand risks and seek proper care2.
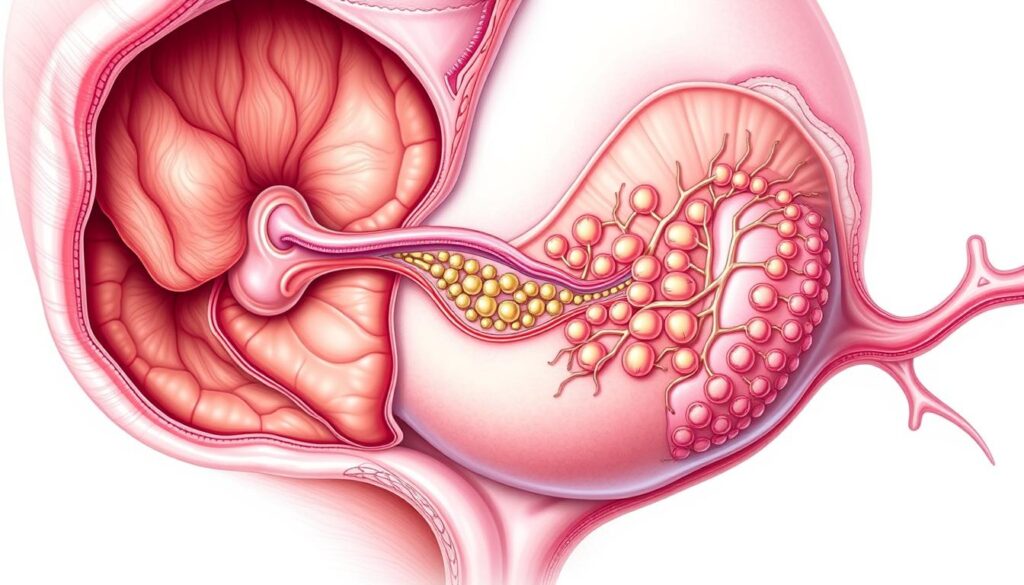
Molar Pregnancy starts with unusual fertilization. The placental tissue grows abnormally instead of supporting a healthy fetus. Two main types exist: complete and partial molar pregnancies1.
Your risk of Molar Pregnancy depends on several factors. Age is important, with higher risks for those under 15 or over 431. Some groups, like Asian women, have higher rates2.
Key Takeaways
- Molar Pregnancy is a rare pregnancy complication involving abnormal placental growth
- Two types exist: complete and partial molar pregnancies
- Age and ethnicity can influence the risk of experiencing a Molar Pregnancy
- Early detection and medical intervention are crucial
- Most cases can be successfully treated with proper medical care
What is a Molar Pregnancy and Its Types
A molar pregnancy is a rare condition where abnormal tissue grows instead of a healthy pregnancy3. It’s caused by a fertilization problem. Knowing the types can help spot potential issues early4.
Molar pregnancies are genetic abnormalities with three main types. Each type affects uterine evacuation and future fertility differently.
Complete Molar Pregnancy
A complete molar pregnancy occurs when sperm fertilizes an empty egg3. This leads to placental tissue growth without a fetus.
- No fetal tissue present
- Abnormal chromosome configuration
- Higher risk of persistent trophoblastic disease (approximately 15%)
Partial Molar Pregnancy
In a partial molar pregnancy, two sperm fertilize one egg4. This creates an abnormal chromosomal makeup. It results in limited, non-viable fetal tissue.
- Minimal fetal tissue formation
- 69 chromosomes instead of normal 46
- Lower risk of persistent disease (around 1%)
Twin Molar Pregnancy
A twin molar pregnancy is extremely rare. It involves a normal fetus developing alongside molar tissue4. This type needs special medical monitoring.
Understanding these pregnancy variations is crucial for early detection and appropriate medical intervention.
Doctors usually detect molar pregnancies during the first ultrasound scan3. This happens between 8-14 weeks. They’ll monitor hCG levels closely and suggest proper treatment.
Symptoms and Risk Factors of Molar Pregnancy
Spotting molar pregnancy signs early is vital for proper care. Knowing the warning signs helps catch potential issues quickly. Gynecologic cancer experts stress the importance of this awareness5.
Key symptoms of molar pregnancy include:
- Vaginal bleeding in the first trimester
- Severe nausea and vomiting
- Pelvic pressure or pain
- Passage of grape-like cysts
Certain factors can raise your molar pregnancy risk. Age plays a big role in this condition6.
- Under 15 years old
- Over 45 years old
- Asian ethnicity
Many worry about fertility after molar pregnancy. The good news is that most women can successfully conceive after treatment. About 80% of women treated for GTN have successful pregnancies later6.
“Knowledge and early detection are your best allies in managing molar pregnancy risks.”
Recurrence is another concern to keep in mind. After one molar pregnancy, your chance of another is about 1%5. This risk jumps to 15-20% after multiple molar pregnancies6.
Doctors often suggest waiting 6-12 months before trying to conceive again. This allows for full recovery and proper monitoring7. Always talk to your doctor about your specific situation and risks.
Diagnosis and Treatment Options for Gestational Trophoblastic Disease
Abnormal Placental Growth requires understanding diagnostic and treatment approaches. Gestational Trophoblastic Disease (GTD) needs a comprehensive medical strategy. This ensures effective management and recovery8.
Initial Diagnosis Methods
GTD detection involves several key diagnostic techniques. Doctors start with ultrasound scans to see uterine abnormalities. They also do blood tests to measure hCG Levels.
Physical exams of reproductive health are part of the process. Quick diagnosis allows for timely intervention and better treatment results9.
- Ultrasound scans to visualize uterine abnormalities
- Blood tests measuring hCG Levels
- Physical examination of reproductive health
Treatment Procedures
The main treatment for GTD is Uterine Evacuation. This can be done through surgical removal of molar tissue. Medication-based tissue elimination is another option.
Chemotherapy may be used for persistent cases. In rare cases, a hysterectomy might be recommended by doctors8.
- Surgical removal of molar tissue
- Medication-based tissue elimination
- Chemotherapy for persistent cases
Post-Treatment Monitoring
Careful follow-up is key after GTD treatment. Your doctor will do regular hCG level checks. They’ll watch for possible tissue recurrence.
You’ll get advice on future pregnancy planning. Patients usually wait 6-12 months before trying to get pregnant again. Close medical supervision is important9.
- Conduct regular hCG level checks
- Monitor for potential tissue recurrence
- Provide guidance on future pregnancy planning
Nearly all women affected by GTN can expect to be cured if managed properly8.
Conclusion
Molar Pregnancy and Gestational Trophoblastic Disease can be complex. These rare conditions need careful medical attention and support10. Most women fully recover and can have successful pregnancies later11.
Early detection is crucial in managing molar pregnancy. Specialized treatment centers have greatly improved patient outcomes. Your fertility after molar pregnancy remains promising10.
Medical advances offer hope and comprehensive care strategies. Many women navigate this experience successfully with proper guidance and support.
Stay informed and work closely with your healthcare team. Regular monitoring and understanding potential complications can help you through this time. Millions of women have overcome molar pregnancy with advanced treatments and supportive care11.
Emotional healing is as important as physical recovery. Seek counseling and join support groups. Give yourself time to process your experience.
Your resilience and medical support are your strongest allies. They’ll guide you towards healing and future family planning.
FAQ
What exactly is a molar pregnancy?
What are the primary symptoms of a molar pregnancy?
Who is at higher risk for developing a molar pregnancy?
How is a molar pregnancy diagnosed?
What treatment options are available for a molar pregnancy?
Can I have a healthy pregnancy after a molar pregnancy?
What is the long-term prognosis for molar pregnancy?
Are molar pregnancies a type of cancer?
Source Links
- Molar pregnancy – Symptoms and causes – https://www.mayoclinic.org/diseases-conditions/molar-pregnancy/symptoms-causes/syc-20375175
- What is molar pregnancy? – https://www.cancerresearchuk.org/about-cancer/gestational-trophoblastic-disease-gtd/molar-pregnancy/about
- Molar pregnancy – https://www.nhs.uk/conditions/molar-pregnancy/
- What Is a Molar Pregnancy? – https://www.webmd.com/baby/what-is-molar-pregnancy
- Risks and causes of molar pregnancy – https://www.cancerresearchuk.org/about-cancer/gestational-trophoblastic-disease-gtd/molar-pregnancy/risks-causes
- Molar pregnancy – https://patient.info/pregnancy/hydatidiform-mole
- Molar Pregnancy – https://myhealth.alberta.ca/Health/pages/conditions.aspx?hwid=hw165877
- Diagnosis and management of gestational trophoblastic disease: 2021 update – https://pmc.ncbi.nlm.nih.gov/articles/PMC9298230/
- Gestational Trophoblastic Disease Treatment (PDQ®) – https://www.cancer.gov/types/gestational-trophoblastic/hp/gtd-treatment-pdq
- Clinical presentation and treatment outcome of molar pregnancy: Ten years experience at a Tertiary Care Hospital in Dammam, Saudi Arabia – https://pmc.ncbi.nlm.nih.gov/articles/PMC5009886/
- Molar pregnancy with a coexisting living fetus: a case series – BMC Pregnancy and Childbirth – https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-022-05004-3