Immune Thrombocytopenia (ITP) disrupts your body’s blood clotting abilities. This rare disorder causes your immune system to attack healthy platelets. This can lead to bleeding complications1.
ITP affects 2 to 4 people per 100,000 each year. It can occur in both adults and children1. The condition has notable peaks during childhood and among older adults2.
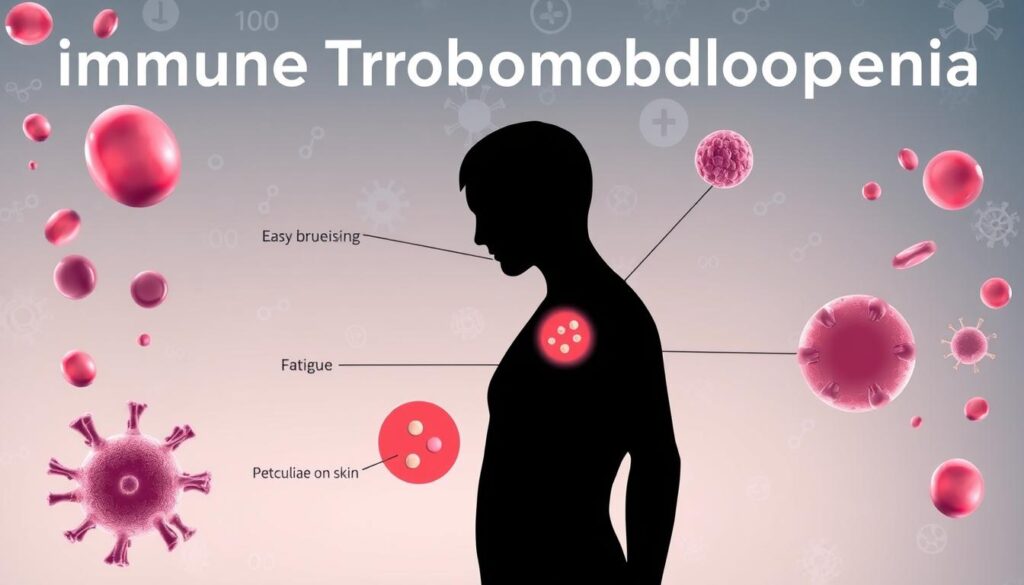
ITP symptoms include easy bruising and frequent nosebleeds. Skin changes may also occur. Severe bleeding happens in 7% to 10% of adult patients1.
Recognizing these signs early is important. It can help you get the right medical care quickly. Talking to a doctor can help you understand your personal risk factors.
Key Takeaways
- ITP is an autoimmune disorder affecting platelet production
- Symptoms include easy bruising and potential bleeding risks
- Affects individuals across different age groups
- Early detection is crucial for effective management
- Medical consultation can help understand individual risk factors
What is Immune Thrombocytopenia (ITP)?
Immune Thrombocytopenia (ITP) is an autoimmune disorder that affects blood clotting. Your immune system attacks platelets, causing a deficiency. This increases your risk of bruising and bleeding3.
Understanding the Basics of ITP
ITP causes low platelet counts in both children and adults. It presents unique challenges for patients.
- Primary ITP affects approximately 9.5 per 100,000 adults3
- The condition can be acute or chronic4
- It impacts approximately 80% of patients as a primary disorder3
How ITP Impacts Your Body
In ITP, your immune system becomes your enemy. Autoreactive antibodies destroy platelets, reducing blood clotting ability.
This can lead to various symptoms, including:
- Easy bruising
- Petechiae (small red or purple spots on the skin)
- Increased bleeding risk
“Understanding ITP is the first step towards effective management and treatment.”
Over 80% of children with ITP recover within six to twelve months4. Adults often develop chronic ITP, with most cases becoming long-term3.
Modern medical treatments offer hope for ITP patients. Steroids, IVIG, and newer therapies can manage platelet deficiency and reduce bleeding risks4.
Common Symptoms of ITP
Immune Thrombocytopenia (ITP) affects your body’s ability to control bleeding. Recognizing these signs helps you spot potential health issues. Seek medical help if you notice these symptoms.
Easy or Excessive Bruising
Bruising is a key sign of ITP. Your body bruises easily, even from small bumps. These bruises can be larger and more frequent than usual.
Low platelet counts cause this easy bruising. They weaken your blood’s natural clotting ability.
Frequent Nosebleeds
Nosebleeds can signal ITP. When platelets drop below 100,000 per microliter, spontaneous bleeding risk increases.
- Unexpected nosebleeds
- Prolonged bleeding duration
- Difficulty stopping nosebleeds
Petechiae and Other Skin Changes
Petechiae are tiny reddish-purple spots on your skin. They show possible bleeding issues. These small hemorrhages can indicate low platelet counts.
Larger skin marks called purpura might also appear. They represent more extensive skin bleeding.
“Recognizing these skin changes early can help manage ITP effectively.”
| Symptom | Description | Potential Risk |
|---|---|---|
| Bruising | Large, frequent bruises | High bleeding risk |
| Petechiae | Tiny red/purple spots | Indicator of low platelets |
| Purpura | Larger skin hemorrhages | Significant bleeding concern |
These symptoms can be scary. However, not all ITP patients experience severe bleeding. Many maintain good platelet levels without intensive treatment5.
Diagnosing Immune Thrombocytopenia
Suspecting immune thrombocytopenia (ITP) requires a thorough diagnostic approach. Your doctor will assess your condition through various medical tests. These evaluations aim to uncover the root cause of low platelet counts.
Blood Tests and Their Importance
Blood tests are key in identifying ITP. A complete blood count (CBC) reveals crucial info about your platelet levels. Doctors focus on your platelet count to check for immune system issues6.
- Peripheral blood smear to confirm platelet deficiency
- Detailed examination of blood cell characteristics
- Assessment of platelet distribution and size
Additional Diagnostic Procedures
Your medical team might suggest more specialized tests. A bone marrow test can help rule out other causes of low platelet count7.
| Diagnostic Test | Purpose |
|---|---|
| Antibody Screening | Detect potential immune system irregularities |
| Bone Marrow Test | Evaluate platelet production and identify underlying issues |
| Viral Investigations | Exclude infectious causes of low platelet count |
Accurate diagnosis is key to developing an effective treatment strategy for immune thrombocytopenia.
Further tests may include glycoprotein-specific antibody screening and antiphospholipid antibody tests. Viral assessments might also be done to get a full picture of your condition6.
Treatments and Management Strategies
ITP management needs a personalized approach based on your symptoms and platelet count. Your doctor may suggest various treatments. These include immunoglobulin therapy to control platelet destruction and improve blood clotting8.
Medications for ITP
Corticosteroids are often used first to reduce platelet destruction. Thrombopoietin receptor agonists like romiplostim can boost platelet production9.
If medications don’t work, your doctor might suggest removing your spleen8.
Lifestyle Modifications
Take steps to prevent bleeding while managing ITP. Wear protective gear during physical activities. Avoid high-impact sports.
ITP patients may have mild to severe bleeding issues. Understanding your risk is important8.
When to Seek Medical Help
Stay alert about your health. Get immediate medical help for uncontrolled bleeding or severe bruising. Watch for signs of internal bleeding.
Regular check-ups with a blood doctor are key. They’ll monitor your condition and adjust treatment as needed9.
FAQ
What is Immune Thrombocytopenia (ITP)?
Who can develop ITP?
What are the common symptoms of ITP?
How is ITP diagnosed?
What treatments are available for ITP?
Can lifestyle changes help manage ITP?
When should I seek immediate medical attention?
Is ITP a life-threatening condition?
Source Links
- Information for Healthcare Professionals about ITP – https://www.understandingitp.com/hcp/en-us/understanding-itp
- Immune Thrombocytopenia – PMC – https://pmc.ncbi.nlm.nih.gov/articles/PMC3672858/
- Pathogenesis and Therapeutic Mechanisms in Immune Thrombocytopenia (ITP) – https://pmc.ncbi.nlm.nih.gov/articles/PMC5332920/
- Boston Children’s Hospital – https://www.childrenshospital.org/conditions/immune-thrombocytopenia-itp
- Immune thrombocytopenia (ITP) – Symptoms and causes – https://www.mayoclinic.org/diseases-conditions/idiopathic-thrombocytopenic-purpura/symptoms-causes/syc-20352325
- How do we diagnose immune thrombocytopenia in 2018? – https://pmc.ncbi.nlm.nih.gov/articles/PMC6245958/
- Laboratory Studies, Imaging Studies, Histologic Findings – https://emedicine.medscape.com/article/202158-workup
- How we treat primary immune thrombocytopenia in adults – Journal of Hematology & Oncology – https://jhoonline.biomedcentral.com/articles/10.1186/s13045-023-01401-z
- Approach Considerations, Thrombopoietin Receptor Agonists, Treatment in Children – https://emedicine.medscape.com/article/202158-treatment