Horner syndrome is a rare brain disorder affecting one side of your face and eye1. It disrupts your nervous system, causing changes in your looks and eye function2. This condition can signal serious health issues needing quick attention.
Horner syndrome can stem from strokes, brain tumors, or spinal cord injuries1. It can affect people of all ages, making it a tricky brain problem2.
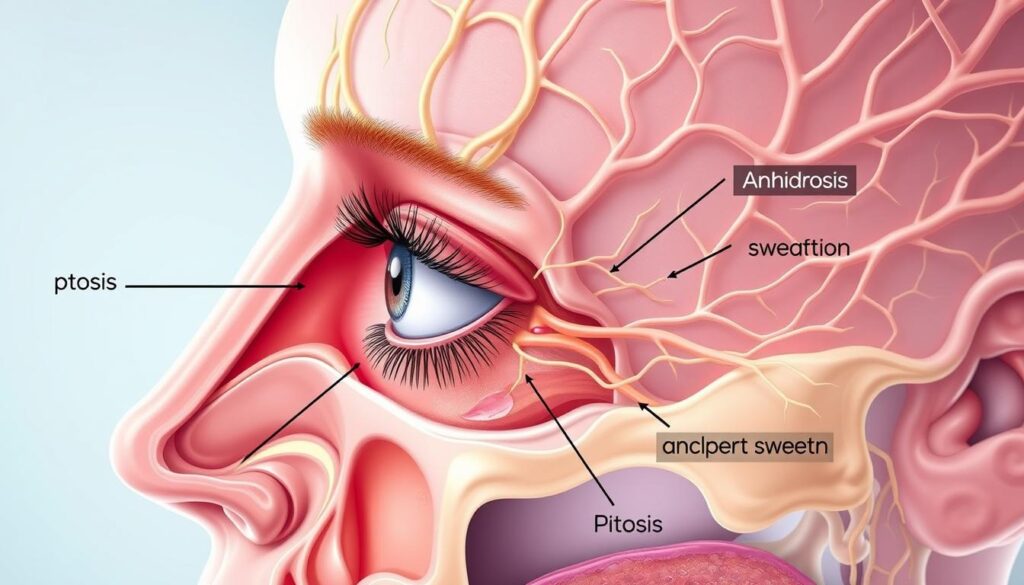
This condition can change your eye and face features noticeably. You might see a smaller pupil, droopy eyelid, or less sweating on one side3. Some patients even have different colored eyes, especially in cases present at birth1.
Key Takeaways
- Horner syndrome is a rare neurological condition affecting facial symmetry
- The syndrome can result from multiple underlying medical conditions
- Symptoms may include pupil changes, eyelid drooping, and reduced sweating
- Diagnosis requires comprehensive medical evaluation
- Treatment focuses on addressing the root cause of the syndrome
What is Horner Syndrome and Its Key Symptoms
Horner syndrome is a rare neurological condition affecting the nervous system and facial appearance. It impacts one side of the face, creating distinctive changes4. About 1 in 6,000 people experience this intriguing neurological phenomenon4.
Recognizing key symptoms can help identify this condition early. The syndrome typically shows several characteristic signs:
- Miosis (a persistently small pupil) on the affected side
- Ptosis (drooping of the upper eyelid)
- Anhidrosis (reduced or absent sweating)
- Enophthalmos (a subtle sunken appearance of the eye)
Common Signs of Facial Involvement
Horner syndrome causes unique facial characteristics. The most noticeable features include different pupil sizes (anisocoria) and a slightly raised lower eyelid5.
Children under one year old might have a lighter iris color in the affected eye5.
Additional Symptoms to Watch For
Some people may experience changes in facial color during physical activity or emotional responses. Symptoms can be hard to spot, especially subtle ones like ptosis and anhidrosis5.
Early recognition of these symptoms can be crucial for proper medical evaluation and potential treatment.
Risk factors for Horner syndrome include nerve pathway disruptions. These can happen through various means4:
- Injuries to sympathetic nerves
- Tumors in specific glands
- Certain infections
- Surgical complications
Often, doctors can’t find a specific treatable cause4. Interestingly, about half of those with miosis may see their pupils return to normal over time4.
Understanding the Causes of Horner Syndrome
Horner syndrome stems from damage to your sympathetic nervous system. This damage can occur at various points along its neural pathway6. Knowing these origins helps doctors diagnose and treat the condition effectively.
The syndrome can result from multiple underlying conditions. Each condition affects different neurological regions:
- First-order neuron damage potentially caused by:
- Stroke
- Tumors
- Spinal column cysts
- Second-order neuron issues might involve:
- Apical lung tumor
- Chest cavity surgery
- Aortic damage
- Third-order neuron problems could include:
- Carotid artery dissection
- Skull base tumors
- Cluster headaches
In children, Horner syndrome often has unique causes. These can include brachial plexus injury during birth, congenital aortic defects, or neuroblastoma7.
“Not all cases have a definitive explanation. Some remain idiopathic, with no identifiable root cause.” – Neurological Research Institute
The origins of Horner syndrome are diverse. Early detection is key to understanding its triggers. A thorough medical evaluation is crucial for managing the condition67.
Diagnosis and Treatment Options
Horner syndrome requires thorough diagnostic procedures and targeted treatment strategies. Your doctor will evaluate your symptoms to determine the best approach. Effective management hinges on accurate diagnosis and tailored care.
Diagnosing Horner syndrome can be complex. Doctors use various techniques to find the underlying cause. They focus on detecting anisocoria and investigating potential neurological issues through advanced medical imaging8.
Diagnostic Procedures
Healthcare experts use several methods to confirm Horner syndrome:
- Comprehensive physical examination
- Detailed eye assessment
- Specialized nerve function tests
- Imaging studies including CT and MRI scans
Interestingly, 35-40% of Horner syndrome cases have an unknown origin9. This fact highlights the need for thorough medical investigation.
Treatment Approaches
Treatment mainly targets the underlying medical condition. In some cases, doctors might consider sympathectomy for managing specific symptoms. This procedure can help with heterochromia or nerve-related complications8.
The key to successful management lies in identifying and treating the root cause of the syndrome.
| Diagnostic Method | Purpose |
|---|---|
| Nerve Conduction Studies | Assess nerve functionality |
| Blood Tests | Rule out systemic conditions |
| Imaging Scans | Identify potential neurological issues |
Horner syndrome can be challenging to manage. However, modern medical approaches offer hope for effective treatment. With proper care, patients can expect improved quality of life9.
Conclusion
Horner syndrome requires a holistic approach to neurological health. Early detection can greatly improve patient outcomes. Keep an eye out for facial flushing, neck pain, and headaches1011.
Horner syndrome is rare, affecting about 1 in 6,000 people worldwide10. Modern tests provide more accurate diagnosis methods1011. While 65% of cases have known causes, some remain unexplained12.
Experts recommend thorough evaluation when symptoms appear. Your doctor may look for neurological lesions, tumors, or trauma1211. Persistent neck pain or unusual facial symptoms need careful investigation.
Personalized care is key in managing Horner syndrome. Stay engaged with your health journey. Keep talking openly with your healthcare team. Learn about your unique neurological profile.
FAQ
What is Horner Syndrome?
What are the main symptoms of Horner Syndrome?
What causes Horner Syndrome?
How is Horner Syndrome diagnosed?
Can Horner Syndrome be treated?
Is Horner Syndrome dangerous?
Can children develop Horner Syndrome?
Are there any long-term effects of Horner Syndrome?
Source Links
- What Is Horner Syndrome? – https://www.verywellhealth.com/horner-syndrome-overview-4176967
- Horner’s Syndrome: Causes, Symptoms, and Treatments – https://www.healthline.com/health/horners-syndrome
- Horner’s syndrome – https://patient.info/doctor/horners-syndrome
- Horner’s syndrome: Overview, symptoms, and more – https://www.medicalnewstoday.com/articles/horners-syndrome
- Horner’s Syndrome – https://uthealthaustin.org/conditions/horners-syndrome
- Horner syndrome-Horner syndrome – Symptoms & causes – Mayo Clinic – https://www.mayoclinic.org/diseases-conditions/horner-syndrome/symptoms-causes/syc-20373547
- Horner syndrome – https://www.mountsinai.org/health-library/diseases-conditions/horner-syndrome
- Horner Syndrome – EyeWiki – https://eyewiki.org/Horner_Syndrome
- Horner Syndrome – https://www.webmd.com/eye-health/horner-syndrome
- Horner’s Syndrome Following COVID-19 Infection and Treatment | Published in CRO (Clinical & Refractive Optometry) Journal – https://clinicaloptometry.scholasticahq.com/article/36745-horner-s-syndrome-following-covid-19-infection-and-treatment
- The Radiology Assistant : Horner syndrome – https://radiologyassistant.nl/head-neck/horners-syndrome-1
- Horner syndrome: clinical perspectives – PMC – https://pmc.ncbi.nlm.nih.gov/articles/PMC5398733/