A pneumothorax, or collapsed lung, can disrupt normal breathing. It happens when air leaks between your lung and chest wall. This can cause chest pain and make it hard to breathe1.
Young men are more likely to get primary spontaneous pneumothorax. Tall young men with fast-growing chests are at higher risk1. Long-term smoking also greatly increases the chance of getting pneumothorax2.
Genes play a big role in pneumothorax risk. Some people with certain gene changes are more likely to get it1. Scientists are still studying why some lungs are more prone to collapse1.
Key Takeaways
- Pneumothorax can cause sudden chest pain and breathing difficulties
- Young men are more susceptible to spontaneous pneumothorax
- Genetic mutations can increase risk of lung collapse
- Smoking significantly elevates pneumothorax risk
- Prompt medical evaluation is critical for proper treatment
What Is Pneumothorax and How Does It Affect Your Lungs
Pneumothorax, or lung collapse, happens when air enters between your lung and chest wall. This air leak disrupts normal breathing and lung function. It’s a serious respiratory condition that needs prompt attention34.
Knowing about pneumothorax helps spot potential health risks. It can impact your breathing in various ways. This condition may cause respiratory distress and make normal breathing difficult4.
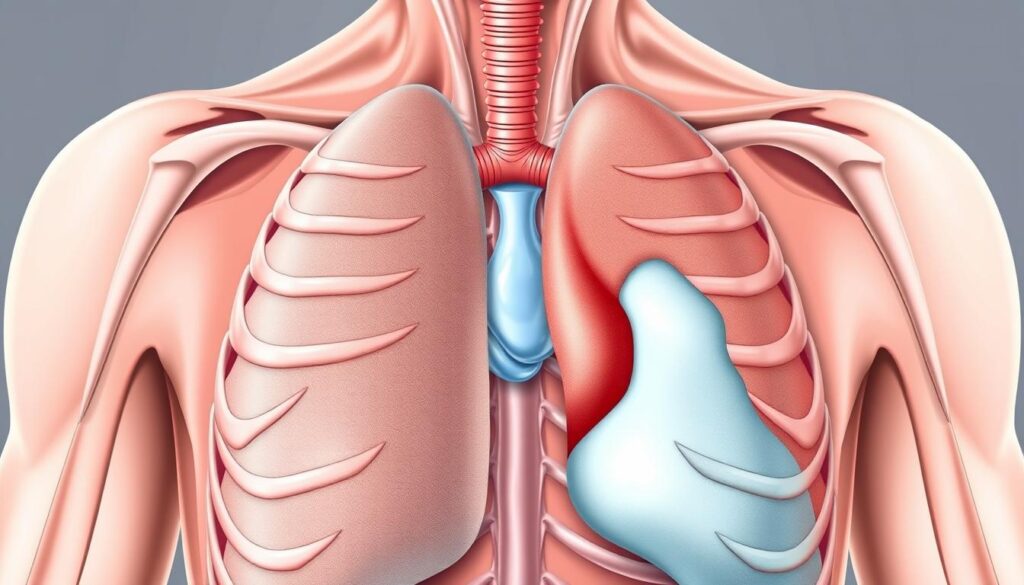
Understanding the Anatomy of a Collapsed Lung
Air in the pleural space creates pressure, stopping your lung from expanding fully. This can cause partial or complete lung collapse. It also reduces lung capacity and oxygen absorption.
- Partial or complete lung collapse
- Reduced lung capacity
- Decreased oxygen absorption
Types of Pneumothorax
Different types of pneumothorax affect you in unique ways:
- Primary Spontaneous Pneumothorax (PSP): Typically occurs in young, tall males aged 10-303
- Traumatic Pneumothorax: Caused by injuries from sports, accidents, or medical procedures4
- Tension Pneumothorax: A life-threatening condition requiring immediate treatment4
Impact on Respiratory Function
Pneumothorax can severely disrupt your breathing. Patients might feel acute chest pain and shortness of breath. It can reduce vital capacity by up to 33%3.
Oxygen levels may also drop in some cases3.
- Acute chest pain
- Shortness of breath
- Reduced vital capacity by up to 33%3
- Potential oxygen level drops3
Understanding the signs and symptoms of pneumothorax can be crucial for timely medical intervention.
If you think you have a lung collapse, get medical help right away. Quick action prevents complications and ensures proper treatment4.
Common Causes and Risk Factors of Pneumothorax
Knowing what causes pneumothorax helps you spot risks and avoid lung problems. A collapsed lung doesn’t just happen. There are key factors that lead to it.
Men face higher risks of pneumothorax than women5. It often affects people aged 20 to 40. Tall and slim individuals are more likely to get it5.
- Chest injuries (blunt or penetrating trauma)
- Underlying lung disease such as COPD
- Smoking-related lung damage
- Genetic predisposition
- Previous lung complications
Smoking greatly ups your risk of pneumothorax. Heavy smokers are 102 times more likely to get a collapsed lung than non-smokers6.
Each year, 7 in 100,000 men and 1 in 100,000 women get pneumothorax6. These numbers show how common it is.
“Your lifestyle and medical history play crucial roles in pneumothorax development.” – Respiratory Health Experts
Medical procedures and machines can cause lung issues. People with chronic lung diseases like COPD face higher risks. About 26 in 100,000 COPD patients get pneumothorax6.
Knowing these risks helps you protect your lungs. You can take steps to reduce lung disease problems.
Diagnosis and Treatment Options for Collapsed Lung
Pneumothorax recovery requires understanding diagnostic and treatment options. Your medical journey will involve evaluation and targeted interventions. These steps are crucial for addressing your collapsed lung effectively.
Medical Evaluation Methods
Diagnosing a collapsed lung needs precise medical imaging. Your doctor will order chest X-rays, ultrasound, or CT scans to assess lung collapse7. These tests help determine the pneumothorax size and severity.
Imaging results guide the treatment strategy. They provide crucial information for your healthcare team to plan effectively.
Available Treatment Approaches
Treatment for pneumothorax depends on your specific condition. Minor cases might allow your lung to re-inflate naturally over weeks7.
More serious situations may need different interventions. These can include needle aspiration or chest tube insertion.
- Needle aspiration to remove excess air
- Chest tube insertion to relieve lung pressure
- Non-surgical repair techniques like pleurodesis
- Thoracic surgery for persistent or recurring cases7
Recovery Timeline and Process
Pneumothorax recovery typically takes 1-2 weeks. During this time, avoid heavy lifting and jarring activities8. About 75-80% of patients fully recover without recurrence after proper treatment8.
Your commitment to following medical advice is key to a successful recovery.
| Treatment Option | Recommended For | Recovery Time |
|---|---|---|
| Observation | Minor air leak | 2-3 weeks |
| Chest Tube | Moderate lung collapse | 1-2 weeks |
| Surgical Intervention | Recurrent pneumothorax | 4-6 weeks |
Note: Always consult your healthcare professional for personalized medical advice regarding pneumothorax treatment.
Conclusion
Lung health is vital, and knowing about pneumothorax management can greatly improve respiratory care. Primary spontaneous pneumothorax occurs more often in males than females. Smoking increases the risk of pneumothorax by up to nine times9.
Medical treatments for pneumothorax have shown good results. Needle aspiration and chest drain insertion are equally effective, with success rates of 62-68%. However, the condition may return in 22-31% of cases within two years9.
Studies continue to improve our understanding of respiratory care. During the COVID-19 pandemic, a small number of patients developed spontaneous pneumothorax. This shows the need for thorough medical monitoring10.
Stay informed and work with healthcare professionals to manage your lung health. This approach can help reduce potential risks and improve overall well-being.
For more details, check out the research on pneumothorax management. Talk to medical experts to create a personalized respiratory care plan.
FAQ
What exactly is a pneumothorax?
What are the main symptoms of a pneumothorax?
Who is at higher risk for developing a pneumothorax?
How is pneumothorax diagnosed?
What are the treatment options for pneumothorax?
How long does recovery take?
Can pneumothorax be life-threatening?
How can I prevent pneumothorax?
Source Links
- Primary spontaneous pneumothorax: MedlinePlus Genetics – https://medlineplus.gov/genetics/condition/primary-spontaneous-pneumothorax/
- Pneumothorax (Collapsed Lung): Symptoms, Causes, and More – https://www.healthline.com/health/collapsed-lung
- Pneumothorax – PMC – https://pmc.ncbi.nlm.nih.gov/articles/PMC3982243/
- Pneumothorax – St Vincent’s Lung Health – https://www.svhlunghealth.com.au/conditions/pneumothorax
- Pneumothorax – Symptoms and causes – https://www.mayoclinic.org/diseases-conditions/pneumothorax/symptoms-causes/syc-20350367
- Pneumothorax – StatPearls – NCBI Bookshelf – https://www.ncbi.nlm.nih.gov/books/NBK441885/
- Symptoms, Diagnosis and Treating Pneumothorax – https://www.lung.org/lung-health-diseases/lung-disease-lookup/pneumothorax/symptoms-diagnosis-treatment
- Pneumothorax (Collapsed Lung) – https://www.webmd.com/lung/what-is-a-collapsed-lung
- Pneumothorax: an update – PMC – https://pmc.ncbi.nlm.nih.gov/articles/PMC2600088/
- Pneumothorax in COVID-19 disease- incidence and clinical characteristics – Respiratory Research – https://respiratory-research.biomedcentral.com/articles/10.1186/s12931-020-01504-y