Bacterial vaginosis (BV) is a common vaginal infection affecting intimate health. It impacts about 35% of people with vaginas, with higher rates among Black individuals1. Understanding BV is key for maintaining vaginal wellness and avoiding complications.
Many women might not know they have BV. Half of those affected show no symptoms, making detection tricky without a medical exam1. BV discharge can be thin, white, gray, or green, often with a fishy smell.
BV isn’t sexually transmitted, but sex can increase your risk. Sexually active people, especially those with multiple partners, are more prone to this infection1. Your lifestyle and hygiene habits play a big role in preventing and managing BV.
Key Takeaways
- Bacterial vaginosis affects approximately 35% of individuals with a vagina
- Many people with BV may not experience noticeable symptoms
- Sexual activity can increase the risk of developing BV
- BV is not a sexually transmitted infection
- Proper vaginal health management is crucial for prevention
Understanding Bacterial Vaginosis
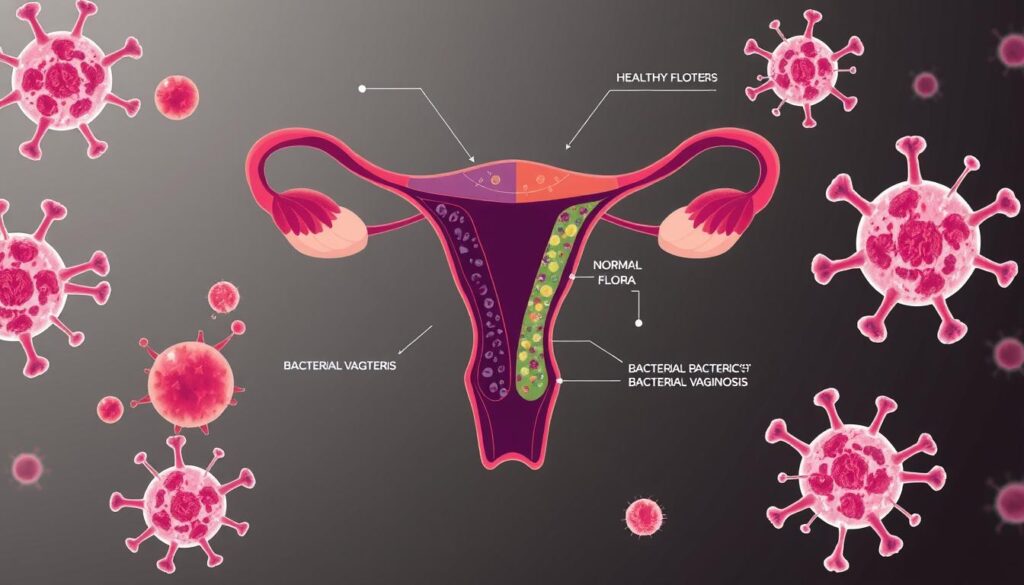
Bacterial vaginosis (BV) is a common intimate health issue affecting women worldwide. It happens when the vagina’s natural bacterial balance gets disrupted. This disruption can lead to bacterial overgrowth and potential complications2.
What Exactly Is Bacterial Vaginosis?
BV is the most common vaginal condition in women aged 15-443. It occurs when normal lactobacilli decrease, allowing other bacteria to grow rapidly. This pH change creates an environment where harmful bacteria thrive2.
Recognizing the Symptoms
Not all women show signs of BV, making it hard to spot. However, some may experience noticeable symptoms.
- Thin, grayish-white discharge
- Unusual fishy odor
- Vaginal itching
- Burning during urination
“Understanding your body’s signals is key to maintaining vaginal health.”
Common Myths and Misconceptions
| Myth | Reality |
|---|---|
| BV is an STD | BV is not a sexually transmitted infection |
| Only women with poor hygiene get BV | BV can affect anyone with vaginal bacterial changes |
BV rates vary across different groups. In the U.S., about 30% of women experience BV. African American women have higher rates2.
Women with multiple sexual partners or those who started sex young face higher risks2.
Remember, while BV can be uncomfortable, it’s treatable and manageable with proper medical guidance.
Causes of Bacterial Vaginosis
Bacterial vaginosis (BV) stems from a complex mix of biological and lifestyle factors. These factors disrupt the natural balance of bacteria in the vagina4.
Factors That Increase Risk
Sexual activity, especially with multiple partners, raises the risk of BV5. Gardnerella vaginalis bacteria can upset the vaginal balance. This makes some women prone to repeated bouts of vaginosis4.
- Multiple sexual partners
- Lack of condom use
- Frequent douching
- Hormonal changes
The Role of pH Balance
A healthy vagina needs the right pH balance. When this balance shifts, harmful bacteria can grow5. An alkaline pH creates ideal conditions for bacterial overgrowth.
Lifestyle Choices That Contribute
Some habits can raise your risk of BV. Douching, using scented products, and unsafe sex can upset your natural balance5. Recurring symptoms may need antibiotic treatment to restore balance.
Protecting your vaginal health requires understanding and mindful choices.
Women with recurring vaginosis should seek professional medical advice. A doctor can offer personalized guidance and long-term management strategies4.
Treatment and Management Options
Bacterial vaginosis requires a targeted approach to restore vaginal health. Antibiotic treatment is the main method for managing this condition. Your doctor can prescribe oral or topical medications to effectively treat the infection67.
Be aware that vaginosis often returns within 3 to 12 months after treatment7. It’s vital to finish all prescribed antibiotics, even if you feel better. Research shows probiotics aren’t very effective in preventing recurring bacterial vaginosis7.
Prevention is key in managing this condition. Avoid douching, using vaginal sprays, or having sex during treatment. Choose breathable cotton underwear and unscented hygiene products for a healthy vaginal environment.
If symptoms persist or recur often, talk to your doctor. They can provide a thorough evaluation and create a personalized treatment plan7. Untreated bacterial vaginosis can increase your risk of sexually transmitted infections6.
Regular check-ups and open talks with your doctor are crucial. These habits help maintain good vaginal health and address concerns quickly.
FAQ
What is Bacterial Vaginosis (BV)?
What are the typical symptoms of Bacterial Vaginosis?
How do I know if I have Bacterial Vaginosis or a yeast infection?
What increases my risk of developing Bacterial Vaginosis?
How is Bacterial Vaginosis treated?
Can Bacterial Vaginosis go away on its own?
How can I prevent Bacterial Vaginosis?
Is Bacterial Vaginosis a sexually transmitted infection?
Can I get Bacterial Vaginosis multiple times?
Is Bacterial Vaginosis dangerous during pregnancy?
Source Links
- Bacterial Vaginosis (BV) – https://www.webmd.com/women/what-is-bacterial-vaginosis
- Bacterial Vaginosis – StatPearls – NCBI Bookshelf – https://www.ncbi.nlm.nih.gov/books/NBK459216/
- About Bacterial Vaginosis (BV) – https://www.cdc.gov/bacterial-vaginosis/about/index.html
- Bacterial vaginosis – https://www.who.int/news-room/fact-sheets/detail/bacterial-vaginosis
- Patient education: Bacterial vaginosis (Beyond the Basics) – https://www.uptodate.com/contents/bacterial-vaginosis-beyond-the-basics/print
- Bacterial Vaginosis – STI Treatment Guidelines – https://www.cdc.gov/std/treatment-guidelines/bv.htm
- Bacterial vaginosis – Diagnosis and treatment – https://www.mayoclinic.org/diseases-conditions/bacterial-vaginosis/diagnosis-treatment/drc-20352285